巨大淋巴结增生症(Castleman病)
2019-10-21 华夏影像诊断中心 华夏影像诊断中心
单发淋巴结肿大一定是转移性淋巴结?多发淋巴结肿大除了转移性淋巴结以外,是不是都要考虑淋巴瘤? C
单发淋巴结肿大一定是转移性淋巴结?多发淋巴结肿大除了转移性淋巴结以外,是不是都要考虑淋巴瘤?
Castleman病(CD,也被称为血管滤泡性纵隔淋巴结增生,血管瘤淋巴结错构瘤和纵隔巨大淋巴结增生症)被称为良性淋巴增生症,可影响纵隔淋巴结,但也可累及肺、胸膜和胸壁、宫颈、肠系膜及腹膜后、脾脏,病因及发病机制不明,多数学者认为它是由淋巴结对不明介质产生少见反应,这种介质最有可能具有病毒的性质。发病年龄和性别无明显差异,少数可向恶性淋巴瘤转化。
Castleman病分型及分类
一、按组织学类型:
①透明血管型(HVV,约占90%):有大量生发中心,散在分布在大量的淋巴细胞和由透明片围成的多毛细血管中间,生发中心是由淋巴细胞同心袖口排列成半透明模式,发育不全的毛细血管后小静脉使病变部位有着血管的外观。
②浆细胞型(PCV):由一层成熟及未成熟的浆细胞组成,生发中心之间混合有免疫母细胞、淋巴细胞和巨噬细胞。
③混合型
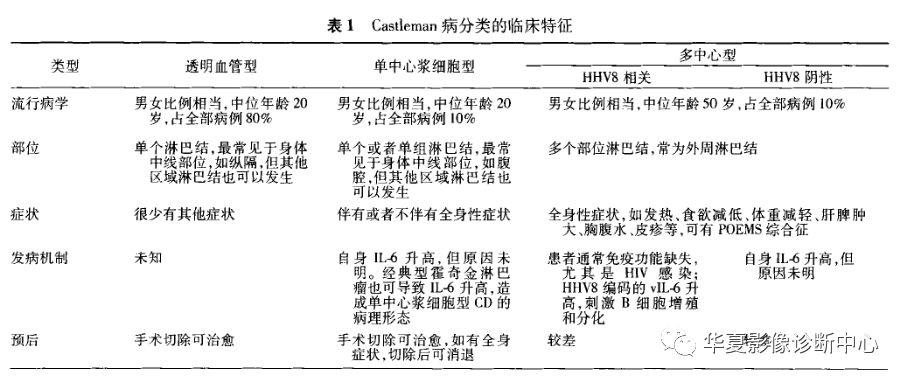
多中心型和浆细胞型的病例有交叉重叠,加上文献及病理书本常常把多中心型也称为浆细胞型,导致临床病理资料和诊断有些混乱。有专家建议把浆细胞型称为单中心浆细胞型Castleman病,以免与多中心型混淆,因此根据其不同临床病理表现分为:透明血管型、单中心浆细胞型、多中心型(HHV8相关或阴性)3种类型。
二、按形态学类型:
①局限型(UCD):96%为透明血管型,预后好,表现为单发,边界清楚的纵隔肿块,或者是合并相关淋巴结肿大的浸润性肿块。
②多中心型(弥漫型 MCD):多为浆细胞型,放化疗及免疫抑制治疗,预后差。表现为弥漫性纵隔或全身淋巴结肿大。
局限型或透明血管型多发生在青壮年,治疗后预后良好,多中心型或浆细胞型比较比较少见(约占10%)通常为多中心发病,表现为全身淋巴结肿大,更常见于老年人和合并有全身性疾病且临床表现为发热、多汗、乏力、贫血、淋巴结肿大、肝脾肿大的患者。
影像学表现
一、X线:局限型或透明血管型表现为孤立性、边界清楚、光滑或分叶状肿块,肺门或中后纵隔最常见,偶尔也可位于主肺动脉窗、后纵隔、胸壁。多中心型或浆细胞型往往累及纵隔多个区域,表现为纵隔弥漫增宽,也可发生弥漫性肺部受累,通常是由淋巴细胞性间质肺炎引起。
二、CT:局限型或透明血管型通常表现为均匀低密度软组织肿块或肿大淋巴结,中心常见粗大钙化灶,由于富含血管,透明血管型的肿大淋巴结增强后有明显均匀强化。多中心型或浆细胞型Castleman病在增强后典型表现为纵隔和肺门区多个轻中度肿大淋巴结,呈轻中度均匀强化。多中心型Castleman病肺部表现通常为淋巴细胞性间质性肺炎,表现为边界不清的小叶中心结节,薄壁囊肿和增厚的支气管血管束和间隔,少见的病变是胸膜下结节、磨玻璃样影、空洞和支气管扩张。
三、MRI:同纵隔脂肪类病变信号相比,Castleman病病灶为低信号,但是T1及T2同骨骼肌的信号相比,为相对高信号,DWI为明显高信号,ADC为低信号,增强扫描同CT。
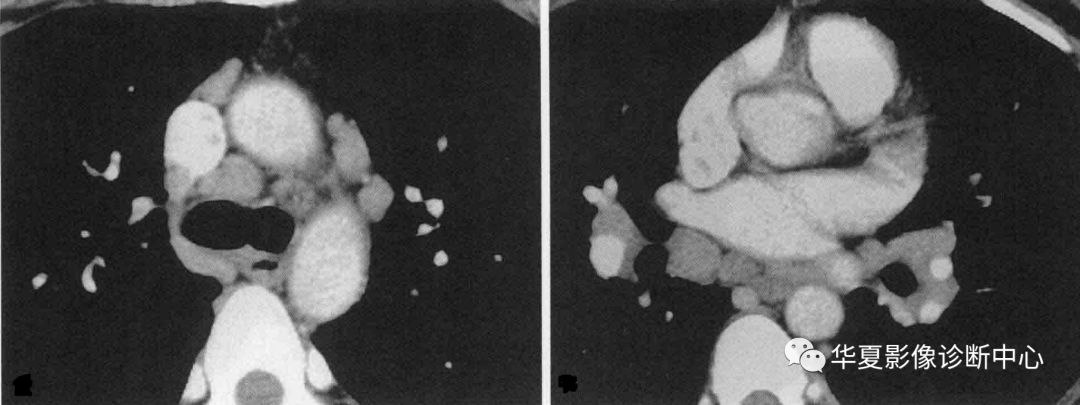 纵隔多中心型Castleman病
纵隔多中心型Castleman病

颈部局限型(透明血管型)Castleman病
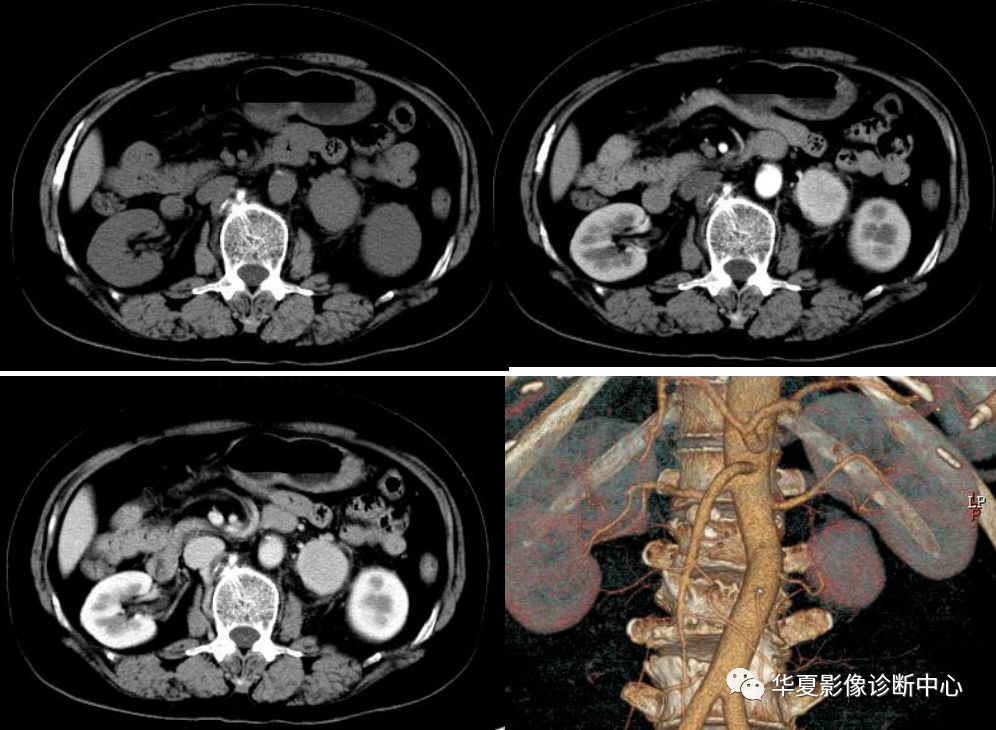
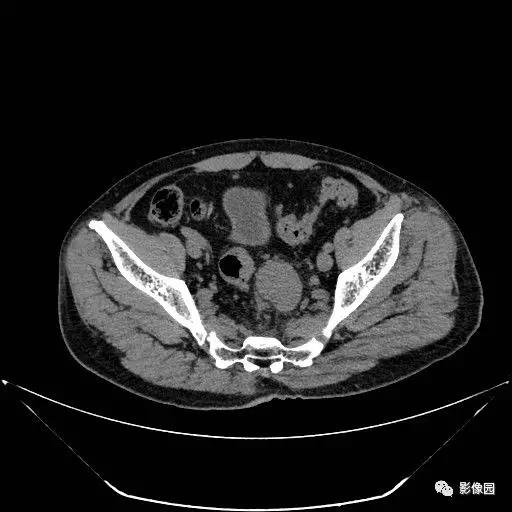
腹部局限型(透明血管型)Castleman病
临床诊断
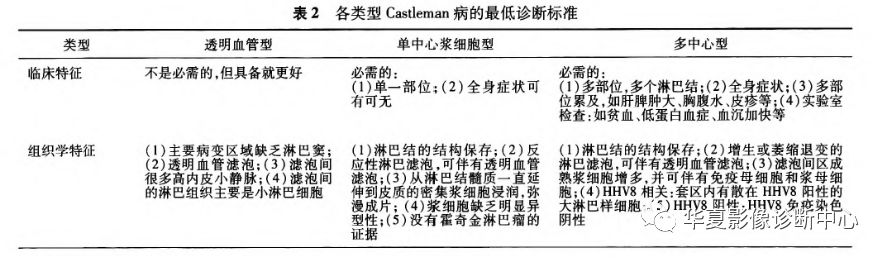
该病病变部位不同,临床表现也复杂多变,确诊主要靠组织病理学诊断。Frizzera,1988年提出CD诊断标准:
(1)局限型的诊断标准,①单一部位淋巴结肿大;②特征性增生性组织病理学改变并除外可能的原发病;③多无全身症状及贫血、红细胞沉降率加快、γ球蛋白增高等异常;④肿物切除后长期生存。
(2) 弥漫型的诊断标准,①具有特征性增生性组织病理改变;②显著淋巴结肿大并累及多处外周淋巴结;③多系统受累表现;④排除已知可能的病因。
必须指出,单凭病理组织学或临床表现可能均难以做出肯定、准确的临床病理诊断,必须把两者结合起来。特别是弥漫型。个别病例不应满足于一次病理学结论,应反复多部位送检,以期尽早明确诊断。
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#AST#
25
#淋巴结#
29
#EMA#
25
#Castleman病#
27
#Cas#
32