静脉动脉体外膜氧合与无肺动脉高压患者的非泵式支持的比较
2022-08-15 刘少飞 MedSci原创
在没有肺动脉高压的患者中,计划中的VA ECMO治疗孤立的BOLT与计划中的非泵式支持相比,有更高的教科书结局的几率。
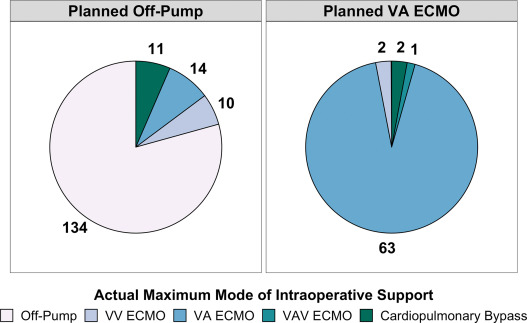
计划中的静脉动脉体外膜氧合(VA ECMO)越来越多地用于双侧正位肺移植(BOLT),对于没有肺动脉高压的患者,可能优于非泵式支持。在这项单一机构的研究中,我们比较了无肺动脉高压或轻度肺动脉高压的受体在计划中使用VA ECMO或非泵支持的BOLT之间的教科书结果率。
研究方法:
我们利用机构和联合器官共享网络(UNOS)的数据进行了一项单中心回顾性队列研究。纳入了2017年1月1日至2021年2月28日期间在杜克大学医院接受隔离式BOLT并计划进行非泵送或VA ECMO支持的成人(年龄≥18岁)患者。随访于2021年11月结束。纳入在2017年1月-2021年2月期间接受隔离式BOLT的无肺动脉高压或轻度肺动脉高压患者,并计划在泵外或VA ECMO支持下进行。教科书上的结果被定义为无术中并发症、30天再干预、30天再入院、移植后住院时间>30天、90天死亡率、30天急性排斥反应、48或72小时内3级主要移植功能障碍、移植后ECMO、7天内气管切开、住院透析、重新插管以及移植后>48小时拔管。使用多变量逻辑回归法比较各组的教科书结果成就。
研究结果:
纳入了237名BOLT患者。68名计划中的VA ECMO和169名计划中的非泵送。14名(20.6%)计划中的VA ECMO和27名(16.0%)计划中的非泵送患者达到了教科书般的结果。在调整了先前的BOLT、肺部分配得分、缺血时间和术中输血后,计划中的VA ECMO与计划中的非泵支持相比,有更高的教科书结局的几率(几率比为3.89,95%置信区间为1.58-9.90,P = 0.004)。
研究结论:
在我们的机构中,在没有肺动脉高压的患者中,计划中的VA ECMO治疗孤立的BOLT与计划中的非泵式支持相比,有更高的教科书结局的几率。需要在多机构的队列中进一步调查,以更好地阐明这一策略的效用。在这项单中心分析中,我们发现,在没有PH值的患者中,计划使用VA ECMO进行孤立的BOLT与计划的非泵送支持相比,有更高的TO实现几率。在非选择性使用VA ECMO作为BOLT期间标准的计划性术中支持策略的热情日益高涨的情况下,我们的研究结果提供了有希望的新证据,以支持更广泛地采用这一策略来改善无PH值患者的围手术期结局。
参考文献:
Halpern SE, Wright MC, Madsen G, Chow B, Harris CS, Haney JC, Klapper JA, Bottiger BA, Hartwig MG. Textbook outcome in lung transplantation: Planned venoarterial extracorporeal membrane oxygenation versus off-pump support for patients without pulmonary hypertension. J Heart Lung Transplant. 2022 Jul 21:S1053-2498(22)02041-1. doi: 10.1016/j.healun.2022.07.015. Epub ahead of print. PMID: 35961827.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#肺动脉高压患者#
46
#动脉高压#
29
#静脉#
30
对ECMO有进一步了解
45
#体外膜氧合#
38