J Am Coll Cardiol:围手术期心肌梗死对血管重建术后结果的影响
2021-05-08 MedSci原创 MedSci原创
经皮冠状动脉介入(PCI)和冠状动脉旁路移植(CABG)手术后,关于围手术期心肌梗死(PMI)的定义有很多。近日,在SYNTAXES试验中,研究人员探究了各种定义的PMI率、与10年全因死亡率的临床相
经皮冠状动脉介入(PCI)和冠状动脉旁路移植(CABG)手术后,关于围手术期心肌梗死(PMI)的定义有很多。近日,在SYNTAXES试验中,研究人员探究了各种定义的PMI率、与10年全因死亡率的临床相关关系以及对5年综合终点的影响,研究结果已发表于J Am Coll Cardiol。
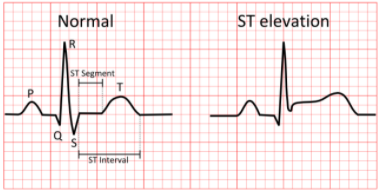
根据SYNTAX、ISCHEMIA和EXCEL试验的定义;MI的第四个通用定义;以及心血管血管造影和介入学会(SCAI)的定义,PMI被划分为手术后48小时内发生的心肌梗死。研究纳入的1800名患者中,有1652名术后有肌酸激酶和/或肌酸激酶心肌带(CK-MB)的患者。通过Cox回归分析了PMI与死亡率之间的关系。
结果,根据SYNTAX和第四个MI的通用定义,PCI组的PMI率分别为2.7%和3.0%,而CABG组为2.4%和2.1%,这两个定义都要求CK-MB升高和心电图显示永久性心肌损伤。根据SCAI或EXCEL定义,PCI(5.7%)和CABG(16.5%)组的PMI率较高。当CK-MB超过10倍ULN时,根据SYNTAX和第四个MI通用定义的PMI与死亡率的关系比EXCEL和SCAI定义的PMI更紧密。这些 "酶驱动事件 "对时间-事件曲线和综合终点的影响在外科研究队列中更大。无论定义如何,PCI术后的PMI与10年的死亡率有关,而它们对CABG术后死亡率的影响仅限于1年。
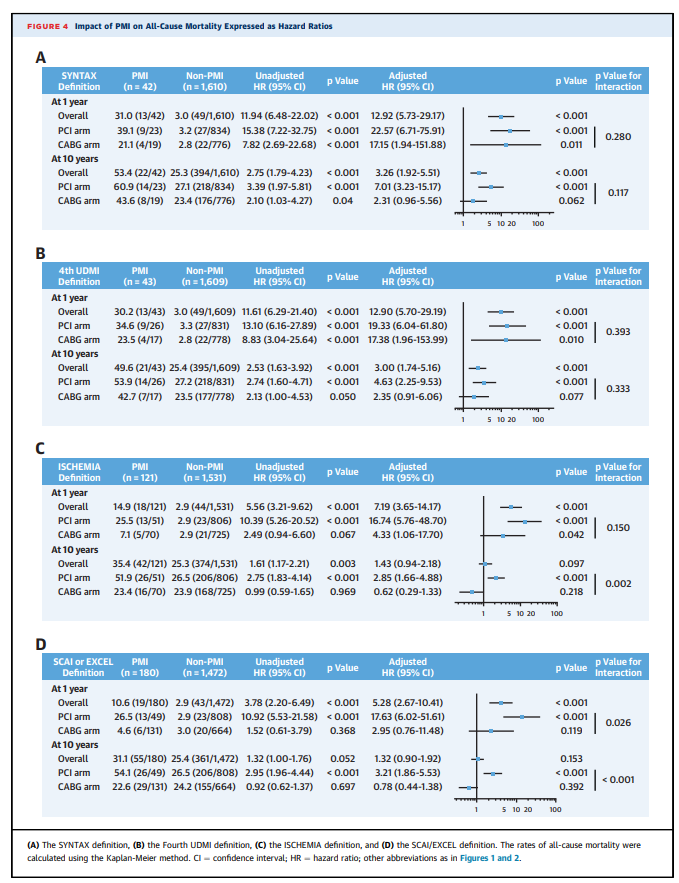
综上所述,该研究结果表明,PMI的发生率高度依赖于其定义,这影响了时间-事件曲线、综合终点以及其致命的预后相关性。
原始出处:
Hironori Hara, et al., Impact of Peri-Procedural Myocardial Infarction on Outcomes After Revascularization. J Am Coll Cardiol. 2020 Oct 6;76(14):1622-1639. doi: 10.1016/j.jacc.2020.08.009.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











#手术期#
45
#Coll#
43
#Cardiol#
37
学习
58
好文章!
65