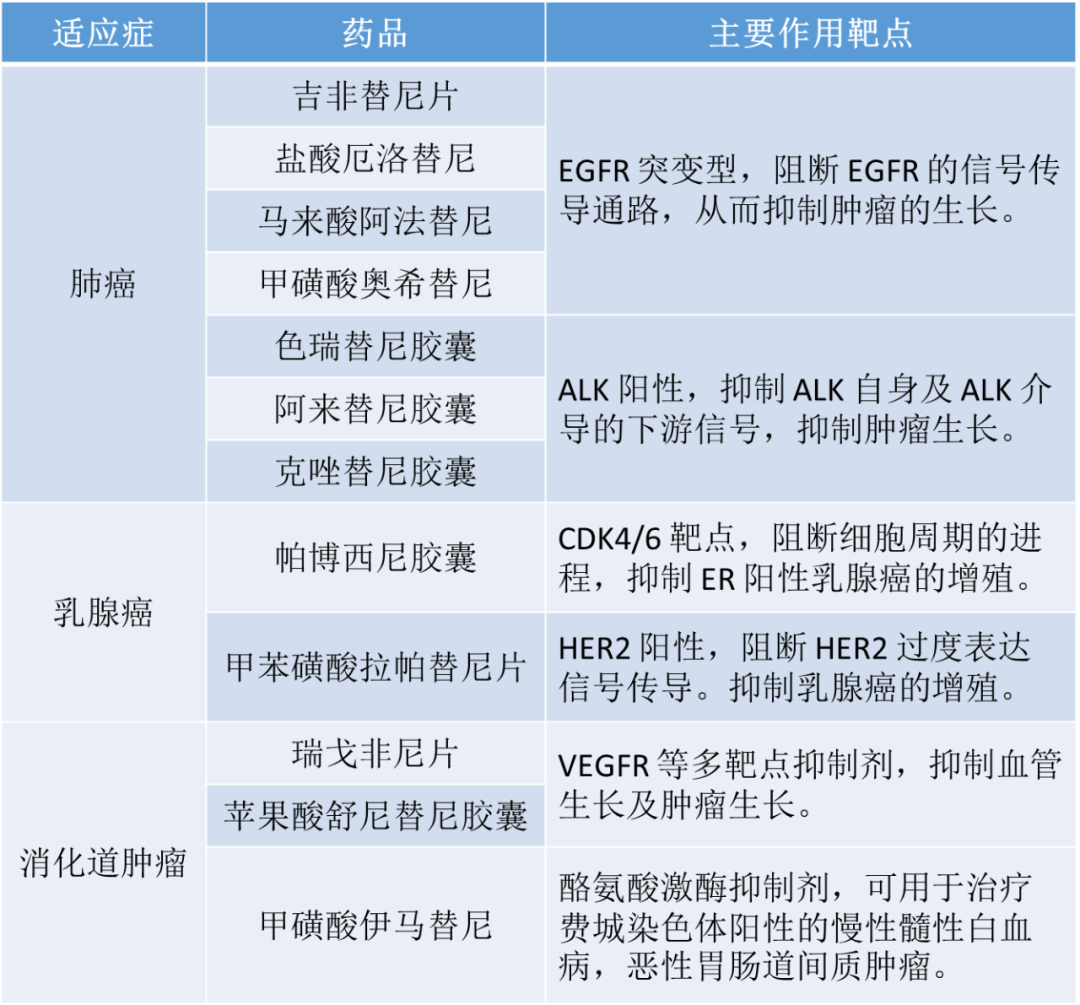
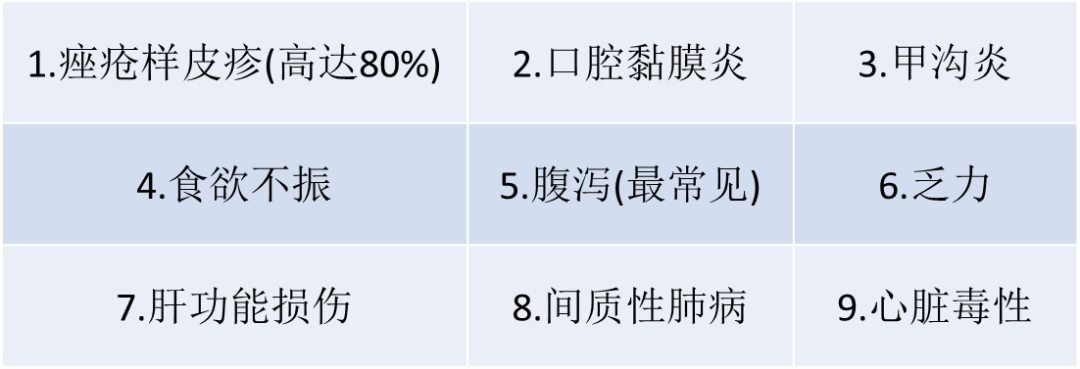
大分子药物:单克隆抗体,如贝伐珠单抗,曲妥珠单抗,此类一般为静脉给药; 小分子靶向药物:包括治疗非小细胞肺癌的 EGFR-TKI 抑制剂(第一代吉非替尼和厄洛替尼、第二代阿法替尼和达克替尼,以及第三代奥西替尼等)和 ALK 抑制剂(第一代克唑替尼,第二代色瑞替尼及第三代劳拉替尼),此类药物一般为口服给药。 严重程度分级: 1 级:<10% 的 BSA 出现丘疹和/或脓疱(伴/不伴瘙痒或触痛); 2 级:10%-30%的 BSA 出现丘疹和/或脓疱(伴/不伴瘙痒或触痛)或社会心理影响或有效日常生活活动受限; 3 级:>30%的 BSA 出现丘疹和/或脓疱(伴/不伴瘙痒或触痛)或日常自我护理受限或合并需口服抗生素的局部双重感染; 4 级:涉及任何 BSA 百分比的丘疹和/或脓疱,伴/不伴瘙痒或触痛,与广泛的双重感染有关并静脉注射抗生素治疗;危及生命。 药物治疗: 1级:根据具体情况,开始使用外用抗生素(1%或2%克林霉素、1%或2%红霉素或1%甲硝唑)、外用类固醇(中等或低规格:0.025% 曲安奈德、0.05% 地奈德、0.05% 阿氯米松乳膏或0.05%丙酸氟替卡松乳膏)和润肤剂治疗; 2级:开始口服抗生素(多西环素 100 mg BID,米诺环素 100 mg BID 或土霉素 500mg BID)4 周以上,如果使用土霉素,则停用外用抗生素使用外用类固醇(中等或低规格:0.025%醋酸曲安奈德、0.05% 地奈德、0.05% 阿氯米松乳膏或 0.05%丙酸氟替卡松乳膏); 3级:开始口服抗生素(多西环素 100mg BID,米诺环素 100mg BID 或土霉素 500mg BID),持续 >4 周如果由于存在黄色结皮、脓性分泌物或皮肤/鼻孔疼痛而怀疑出现感染时,将口服抗生素转换为口服广谱革兰氏阴性菌抗生素治疗>10天;考虑用皮肤拭子进行细菌培养;考虑咨询皮肤科医生继续使用局部类固醇(中等或低强度::曲安奈德 0.025%,地索奈德 0.05%,阿氯米松 0.05% 霜剂,或丙酸氟替卡松 0.05%); 4级:根据医生的临床判断提供额外的管理建议。 患者教育: 第一次用药前,应预防性地使用无香味的润肤霜滋润皮肤,并在整个治疗期间持续使用; 暴露于阳光的部位可能会发生皮肤不良反应或恶化,因此,应避免皮肤晒黑。在暴露在阳光下的情况下,应穿着防护服,并每隔2小时涂抹一次防晒霜[防晒系数(SPF)≥30]; 应避免在淋浴/洗澡期间过度暴露于热水,并避免做浸入热水、洗涤剂或溶剂中的家务。 严重程度分级: 1级:与基线相比,每天排便次数增加<4次; 2级:与基线相比,每天排便次数增加 4-6次; 3级:每天排便次数比基线增加 ≥7 次或尿失禁或日常生活不能自理或住院治疗; 4级:危及生命。 药物治疗: 1级:首次发生腹泻时开始服用止泻药(如洛哌丁胺 4mg),并持续至腹泻停止后12 小时(如有必要,将止泻药提高至最高推荐剂量);脱水的患者可能需要静脉输注液体和电解质。 2级:同1级腹泻管理,开始使用止泻药(如洛哌丁胺 4mg)或考虑使用标准剂量的盐酸地芬诺酯和硫酸阿托品制剂治疗;密切监测患者并考虑静脉补液。 3级:开始止泻药物治疗(盐酸地芬诺酯和硫酸阿托品复方制剂或阿片酊口服治疗);考虑皮下注射 100-150ug 奥曲肽,每日2次;然后增加至每日3次,每次皮下注射 500ug;保持摄入充足的水(2L),或适合时静脉输注液体或电解质;如果在 24 小时内没有改善到2级,或者出现发烧、腹痛等,请考虑住院治疗。 4级:让患者住院,从而获得最大的液体和营养支持;根据医疗人员的临床判断,开始使用抗生素治疗发烧、白细胞增多或明显脱水。 患者教育: 鼓励患者保持足够的饮水,每天喝 8-10 大杯水(2升)以避免脱水; 对于乳糖不耐症患者,为了减少腹泻的影响,应不食用含有乳糖的产品; 而对于排便次数增加的患者,建议少食多餐,选含有香蕉、大米、苹果酱和吐司的低脂饮食方案。 严重程度分级: 1级:无症状或轻度症状; 2级:中度疼痛,不影响口服药物;需调整饮食; 3级:重度疼痛,影响口服药物; 4级:危及生命;需紧急干预。 药物治疗: 1级:无需干预; 2级:可根据医疗人员的判断或根据当地临床实践,使用局部麻醉药或全身麻醉药; 3级:可根据医疗人员的判断或根据当地临床实践,使用局部麻醉药或全身麻醉药推荐局部类固醇冲洗(如地塞米松 0.5mg/5ml,每日漱口4次); 4级:根据医疗人员的临床判断提供额外的管理建议。 患者教育: 应建议患者定期用温水和非药物盐水冲洗,在吃饭时宜喝水,应避免使用含氯己定的口服产品,经常更换牙刷(软毛牙刷),并使用温和的冲洗液或保湿霜; 可能需要营养咨询,从而保持热量摄入; 定期随访中的患者应进行周期性口腔系统性检查,并建议患者出现任何口腔黏膜不适或口腔粘膜外观可见变化应立即报告。 严重程度分级: 1级:指甲皱褶水肿或红斑或角质层破裂; 2级:需要局部干预,或口服干预治疗(如抗生素、抗真菌或抗病毒治疗)或甲褶皱水肿或红斑伴有疼痛或合并分泌物或指甲板分离或日常家务活动受限; 3级:需手术干预或静脉注射抗生素或自我护理能力受限。 药物治疗: 1级:使用外用抗生素(1%克林霉素或1%红霉素)开始治疗,每天用1:1白醋水溶液浸泡手指或脚趾15分钟; 2级:使用外用抗生素(1%克林霉素或1%红霉素)开始治疗,每天用1:1白醋水溶液浸泡手指或脚趾15分钟,每周涂一次硝酸银; 3级:使用外用抗生素(1%克林霉素或1%红霉素)开始治疗,每天用1:1白醋水溶液浸泡手指或脚趾 15 分钟,每周涂一次硝酸银,并根据需要进行外科咨询。 患者教育: 穿舒适、透气的鞋袜; 保持指甲修剪,但避免修剪过度或使用腐蚀性物质修剪指甲; 做家务时应戴手套。 严重程度分级: 1级:累及<10% 的 BSA 且不伴相关的红斑或瘙痒; 2级:累及 10%-30% 的 BSA 且伴有红斑或瘙痒或有效的日常生活活动受限; 3级:累及 >30% 的 BSA 且伴有红斑或瘙痒或自我护理能力受限。 药物治疗: 1级:使用非处方保湿霜或软膏涂抹于面部,每日两次;使用含 12% 乳酸铵(或同等其他成分)乳膏涂抹全身,每日两次; 2级:使用非处方的保湿霜或软膏涂抹于面部,每日两次;使用含 12% 乳酸铵(或同等其他成分)或 6%水杨酸乳膏涂抹全身,每日两次; 3级:使用非处方的保湿霜或软膏涂抹于面部,每日两次;使用含 12% 乳酸铵(或同等其他成分)乳膏涂抹全身,每日两次;局部应用类固醇药物(中等/低强度:曲安奈德 0.025%、地奈德 0.05%、阿氯米松 0.05% 或丙酸氟替卡松 0.05%)用于湿疹部位,每日两次。 患者教育: 用药前,应预防性地使用无香味的润肤霜滋润皮肤,并在整个治疗期间持续使用; 患者应避免在淋浴/洗澡期间过度暴露于热水,并避免做浸入热水、洗涤剂或溶剂中的家务; 暴露于阳光的部位可能会发生皮肤不良反应或恶化,因此,患者应避免皮肤晒黑。对于那些暴露在阳光下的患者,应穿着防护服,并在每隔2小时涂抹一次防晒霜[防晒系数(SPF)≥30]。
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言













#不良反应#
76
#小分子#
40
#分子靶向#
56
#肿瘤药#
54
#抗肿瘤药#
49
学习学习学习学习学习学习学习学习学习学习学习学习学习学习学习学习学习学习学习学习学习学习学习学习学习学习学习
50