AJKD:CKD进展与死亡率的性别差异
2021-01-10 MedSci原创 MedSci原创
与女性相比,男性CKD患者的全因和心血管疾病死亡率更高,CKD进展的风险增加,eGFR下降更陡。
慢性肾脏病(CKD)是全球性的健康问题,其患病率正在不断上升。对于疾病进展和死亡率,已有研究报道了几种类型的性别差异。选择和生存偏倚可能已经影响了先前队列研究的结果。近日,肾脏病学权威杂志Am J Kidney Dis上发表了一篇研究文章,研究人员旨在调查未接受维持性透析的CKD患者CKD进展和死亡率的性别差异。
这项观察队列研究参与者为2010年至2018年期间在瑞典肾脏登记中心(SRR-CKD)确定的患有G3b-5期的CKD成年患者。该研究的结局为进展到CKD时间,定义为CKD至少进展一期或开始肾脏替代治疗(KRT)或死亡。研究人员对eGFR进行了重复评估,并通过累积发病函数法和Fine和Grey模型评估KRT前CKD的进展和死亡率,并将死亡视为竞争性事件。研究人员使用混合效应线性回归模型估计了eGFR斜率的性别差异。
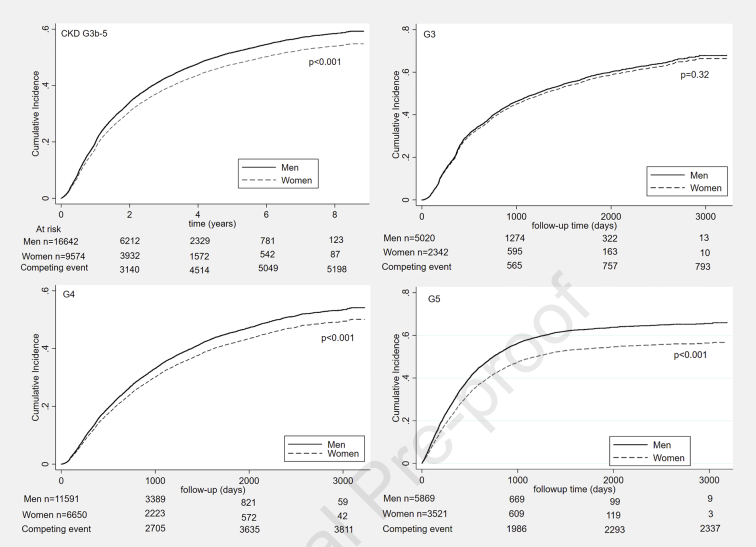
研究人员确认了7388例G3b的CKD患者,18282例G4的CKD患者和9410例G5的CKD患者。总体而言,CKD进展为19.6例患者/100人/年(95%置信区间[CI]为19.2-20.0),死亡的患者为10.1例患者/100人/年(95%CI为9.9-10.3)。女性CKD患者进展风险较低(亚风险比[SHR]为0.88 [0.85-0.92]),全因死亡(SHR为0.90,95%CI为0.85-0.94)和心血管死亡风险(SHR为0.83,95%CI为0.76-0.90)较低。与eGFR斜率上升有关的危险因素包括年龄、性别、蛋白尿和原发性肾脏疾病类型。
由此可见,与女性相比,男性CKD患者的全因和心血管疾病死亡率更高,CKD进展的风险增加,eGFR下降更陡。
原始出处:
Oskar Swartling,et al.CKD Progression and Mortality Among Men and Women: A Nationwide Study in Sweden.Am J Kidney Dis.2021.https://www.ajkd.org/article/S0272-6386(21)00018-4/fulltext
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#CKD进展#
40
谢谢
87
了解
80
学习了谢谢谢
107
学习了谢谢
80
Ajsn流弊
0
学习了谢谢
50
学习了谢谢
53
慢性肾脏病(CKD)是全球性的健康问题,其患病率正在不断上升。
42
#慢性肾脏病#
122