NEJM:Evolocumab 治疗对于认知功能影响研究
2017-08-17 zhangfan MedSci原创
Evolocumab联合他汀类药物不会对患者的认知功能造成影响
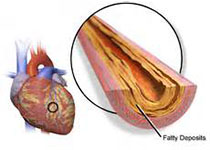
临床研究发现,PCSK9抑制剂或者极低的LDL胆固醇水平与认知障碍相关。近日,研究人员考察了PCSK9抑制剂Evolocumab联合他汀类药物对患者认识功能的影响。
研究人员利用剑桥神经心理学评估药物对患者认知的影响。主要终点为执行功能-空间-工作记忆-策略指标得分(4-28,分数低策略越有效);次要终点为工作记忆得分(0-279, 分数低错误多), 事件记忆(0-70, 分数低,错误少)以及精神运动速度 (100-5100 msec, 速度快表现好)。在试验基线、第24周、每年以及试验结束时进行认知功能评估。
共1204名患者参与研究,平均研究时间19个月。主要终点方面,执行功能-空间-工作记忆-策略指标得分 Evolocumab组?0.21±2.62,对照组?0.29±2.81。次要终点方面,组间无显著差异:工作记忆得分(原始分数变化, Evolocumab组vs对照组-0.52 vs-0.93), 事件记忆( -1.53 vs-1.53),精神运动速度(5.2 vs 0.9 msec)。扩展分析认为LDL胆固醇水平与认知障碍无相关性。
研究认为,Evolocumab联合他汀类药物不会对患者的认知功能造成影响。
原始出处:
Robert P. Giugliano et al.Cognitive Function in a Randomized Trial of Evolocumab. N Engl J Med,August 17, 2017
本文系梅斯医学(MedSci)原创编译整理,转载需授权!
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#mAb#
33
#Evolocumab#
34
谢谢分享,学习了!
50
学习一下
55
安全性的论证,很棒
66