Chest:伴有房颤的脓毒症患者使用苯肾上腺素和去甲肾上腺素后对心率效应的比较
2022-05-26 MedSci原创 MedSci原创
在伴有房颤的脓毒症患者中,与去甲肾上腺素相比,使用苯肾上腺素与心率轻度降低相关。在开始升压时的心率似乎是一个重要的效应调节因子。
心房颤动(AF)是脓毒症常见的并发症。目前尚不清楚α-和β-激动剂去甲肾上腺素和α-激动剂苯肾上腺素是否与伴有房颤的脓毒症患者不同心率之间存在相关性。

近日,呼吸领域权威杂志chest上发表了一篇研究文章,研究人员旨在明确在伴有房颤的脓毒症患者中使用苯肾上腺素和去甲肾上腺素后对心率的影响有何不同?

研究人员利用重症监护医疗信息(MIMIC)-IV数据库,确定了在开始使用去甲肾上腺素或苯肾上腺素时治疗的伴有房颤的脓毒症患者。此外,研究人员采用多变量校正线性回归法评估了在使用苯肾上腺素或去甲肾上腺素开始升压后1小时和6小时的患者心率差异,并评估了心率对疗效的影响,同时,根据基线心率≥110bpm或<110bpm进行了分层。该研究的次要结局包括转换为窦性心律、心动过缓、升压药物使用时间、重症监护室(ICU)和住院时间,以及医院死亡率。研究人员采用间断时间序列的敏感性分析来估计接受苯肾上腺素和去甲肾上腺素治疗的患者平均心率之间的差异。
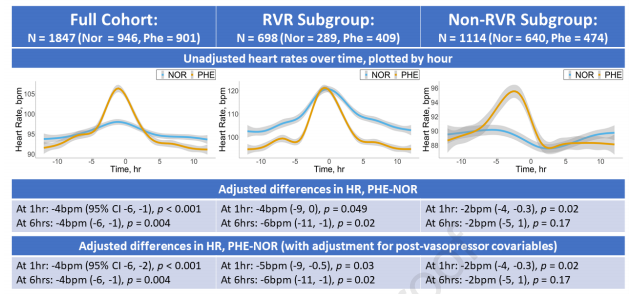
在1847例伴有房颤的脓毒症患者中,946例(51%)患者接受了去甲肾上腺素治疗,901例(49%)患者接受了苯肾上腺素治疗。多变量调整后,苯肾上腺素与1小时(-4bpm[95%CI为-6,-1],p<0.001)和6小时(-4bpm[-6,-1],p=0.004)心率降低相关。与去甲肾上腺素相比,使用苯肾上腺素的患者在给药前心率较高与心率降低幅度较大相关。两组间次要结局无显著差异。探索性分析和敏感性分析结果两组也相似。
由此可见,在伴有房颤的脓毒症患者中,与去甲肾上腺素相比,使用苯肾上腺素与心率轻度降低相关。在开始升压时的心率似乎是一个重要的效应调节因子。但心率适度降低是否与临床结果相关,还需要进一步研究。
原始出处:
Anica C. Law.et al.Comparison of heart rate after phenylephrine versus norepinephrine initiation in patients with septic shock and atrial fibrillation.chest.2022.https://journal.chestnet.org/article/S0012-3692(22)00891-1/fulltext
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言














#Chest#
63
#肾上腺#
54
#EST#
43
#肾上腺素#
74
#脓毒症患者#
37