SMC 批准针对罕见突变晚期肠癌患者的免疫治疗组合(Nivolumab联合ipilmumab)
2021-12-19 Allan MedSci原创
Nivolumab联合ipilmumab已被苏格兰药物联盟 (SMC) 批准为成人患者的治疗选择,用于治疗以前基于氟嘧啶的化疗失败的患者。
Nivolumab联合ipilmumab已被苏格兰药物联盟 (SMC) 批准为成人患者的治疗选择,用于治疗以前基于氟嘧啶的化疗失败的患者。
近日,百时美施贵宝 (BMS) 宣布苏格兰药物联盟 (SMC) 已接受Nivolumab联合ipilmumab作为错配修复缺陷 (dMMR) 或微卫星不稳定性高 (MSIH) 晚期结直肠癌成人的治疗选择,这些患者之前基于氟嘧啶的化学疗法失败后,该疗法供苏格兰NHS使用。
该组患者的特征是罕见的基因突变,称为 MSI-H 或 dMMR,这会影响癌症的生长方式。肠癌是苏格兰的一个重要公共卫生问题,其癌症发病率高于西方世界的大多数其他国家。它是苏格兰男性和女性中第三大最常诊断的癌症,2017 年诊断出约 3,700 例新病例。SMC 建议基于正在进行的 CheckMate-142 研究的数据。
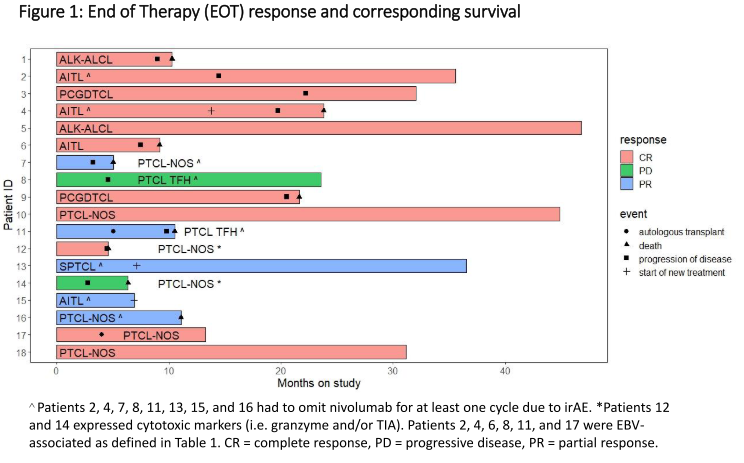
接受治疗的患者的中位年龄为 66 岁(N = 45)。 中位随访时间为 29.0 个月。 客观缓解率和疾病控制率分别为 69%(95% CI,53 至 82)和 84%(95% CI,70.5 至 93.5),完全缓解率为 13%。 未达到中位反应持续时间; 74% 的缓解者在数据截止时有持续响应。24 个月PFS率和OS率分别为 74% 和 79%)。无论基线人口统计学和肿瘤特征如何,包括 BRAF 或 KRAS 突变状态,都观察到了临床获益。在事后分析中,14 名停止治疗且未接受后续治疗的患者中,10 名保持无进展。22% 的患者发生了 3-4 级治疗相关不良事件,13% 的患者因任何级别的治疗相关不良事件而停药。
Nivolumab联合ipilmumab显示出强大而持久的临床益处,并且作为 MSI-H/dMMR mCRC 的一线治疗具有良好的耐受性。
原始出处:
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言

















#治疗组#
40
#SMC#
36
#mAb#
36
#NIV#
31
#罕见#
41