糖尿病人过冬,谨记这9点!
2017-01-17 山东省济南医院糖尿病诊疗中心主任 王建华 医学界内分泌频道
mportant; word-wrap: break-word !important;">保持心态平和据调查,大约50%糖尿病患者存在各种各样的心理问题,许多病人容易出现情绪波动,这种情况在冬季尤为突出。而情绪激动除了能引起交感神经兴奋、血压升高之外,还可促进肝糖原分解,使血糖升高,导致病情加重或降低治疗效果。所以,糖尿病患者要学会控制情绪,尽量减少情绪波动。, 冬天,糖尿病病人抵抗力差,更易发生
冬天,糖尿病病人抵抗力差,更易发生感冒而诱发肺部感染;另外,寒冷会刺激交感神经兴奋,使体内儿茶酚胺类神经递质分泌增加,容易导致血糖及血压升高,诱发心脑卒中;除此之外,严寒还会使外周血管收缩,增加糖尿病足的风险。因此,糖尿病患者在冬季需要做好保健,重点做好以下几点:
一 注意控制饮食
为了抵御冬季寒冷,往往需要靠多吃来增加热量的摄入,而冬季人们户外运动偏少,能量消耗不足,再加上寒冷的天气可使交感神经兴奋,肾上腺素等升糖激素分泌增多,这些因素加在一起使得患者冬季血糖往往较其他季节偏高。因此,在冬季,糖尿病患者要注意控制饮食,少吃多餐,适当运动,如果这样仍难控制血糖,可以在医生的指导下,适当调整降糖药剂量。
二 防止受凉感冒
冬季是呼吸道感染的高发季节,而呼吸道感染也是导致糖尿病酮症酸中毒的常见诱因。为了避免受凉感冒,糖尿病人要做好以下几点:
1、居室经常通风,但室温不宜过低;
2、平时加强锻炼,增强体质;
3、天冷出门前戴好口罩、帽子。
三 取暖须防烫伤
冬天为了御寒,许多病人用暖水袋、暖手宝取暖,但由于糖尿病患者多伴有神经病变,对温度不敏感,很容易发生烫伤,严重者可导致足坏疽,因此,尽量避免采用这类方法取暖。此外,还有些老年病人习惯每天用热水泡脚,为避免烫伤,泡前一定要先用手试水温,最好用手腕去试。水温不要超过40摄氏度,泡脚时间不要超过30分钟。泡完要用干毛巾把脚擦干,特别是脚趾缝。
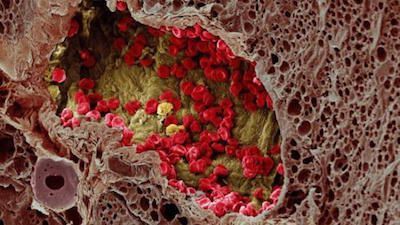
四 加强足部护脚
病程较长的糖尿病人往往合并下肢血管及神经病变,造成脚的末梢循环障碍和感觉迟钝,即使足部受伤也不察觉不到,很容易发展为足坏疽。因此,糖尿病人应特别注意足部保护,穿吸汗、透气性好的棉袜,鞋子要宽松合脚,避免足部外伤及感染。
五 谨防皮肤干燥
冬季天干物燥,常出现皮肤瘙痒,糖尿病人因此引发神经性皮炎甚至湿疹的不鲜见。因此,糖尿病人冬季一定要预防皮肤干燥,特别是小腿及双足,以免破口、皲裂;洗澡、洗脚后须涂抹护肤乳。
六 天冷莫忘喝水
天气寒冷,小便较频。但很多老年人由于口渴中枢不敏感,口渴症状不明显,常常忽视补充水分,导致血粘度升高。一般说来,糖尿病人每天的饮水量不宜低于1500毫升,这样做可以稀释血液,预防心脑血管意外。建议糖尿病人每天早上一起床就要喝杯水,白天多喝,晚饭后少喝,但夜间起夜后要补喝。
七 不宜清晨空腹运动
运动不仅有助于降低血糖、控制体重,也能够增强耐寒能力及机体免疫力。因此,如果没有禁忌证,患者尽量根据自身年龄及身体状况,坚持参加运动(如步行、慢跑、太极拳)。但不提倡晨练,原因有三:
一是早晨气温很低,导致人体产生应激反应,使得血糖升高;
二是清晨空腹锻炼,有低血糖风险;
三是寒冷会使血管骤然收缩,易诱发脑卒中。
因此,户外运动时间最好选在早、晚饭后进行。另外,空气污浊的雾霾天不宜室外活动,可选择在室内运动(散步或做操)。
八 气温骤变勤测血糖
冬日气温时常变动很大,动辄大风降温10摄氏度以上。对于广大糖尿病人来说,这种变化很可能带来血糖波动。因此,当遇到气温骤变或生活方式调整(如增加运动量、减少饭量等)时,要密切监测血糖,以掌握病情变化。
九 保持心态平和
据调查,大约50%糖尿病患者存在各种各样的心理问题,许多病人容易出现情绪波动,这种情况在冬季尤为突出。而情绪激动除了能引起交感神经兴奋、血压升高之外,还可促进肝糖原分解,使血糖升高,导致病情加重或降低治疗效果。所以,糖尿病患者要学会控制情绪,尽量减少情绪波动。
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言













谨记了,谢谢
59
继续学习中
66
切记不要
63
学到很多呦,我要发盆友圈
72
谢谢!学习!
62