CELL: 复旦大学樊嘉团队揭示早期复发肝癌的单细胞景观
2020-12-27 haibei MedSci原创
我们对于与肝癌术后快速复发相关的分子机制仍知之甚少。对肿瘤复发的深入探索可以提高我们对肿瘤发生和进展相关机制的理解,有助于发现更有效的HCC治疗策略,包括免疫疗法。
肝癌是全球癌症相关死亡的第四大原因。肝细胞癌(HCC)是最主要的肝癌形式,占患者的75%-85%。对于肝癌,手术切除是目前最有效的治疗方法,具有治愈潜力。然而,肿瘤复发的高发生率(术后5年50%-70%)阻碍了生存率的提高。此外,术后2年内的早期复发占复发HCC病例的70%,这种复发很少可以治疗,并且与不良生存期相关。
但是目前,我们对于与肝癌术后快速复发相关的分子机制仍知之甚少。对肿瘤复发的深入探索可以提高我们对肿瘤发生和进展相关机制的理解,有助于发现更有效的HCC治疗策略,包括免疫疗法。
最近,来自复旦大学的樊嘉及其合作团队共同剖析了18例原发性或早期复发HCC病例的1.7万个细胞的转录组。
在两个独立的队列中,与原发肿瘤相比,早期复发肿瘤的调节性T细胞水平降低,树突状细胞(DCs)增加,浸润性CD8+T细胞增加。值得注意的是,复发肿瘤中的CD8+T细胞过度表达KLRB1(CD161),并表现出类似先天性的低细胞毒性状态,克隆扩张程度低,这不同于原发性HCC中观察到的经典耗竭状态。
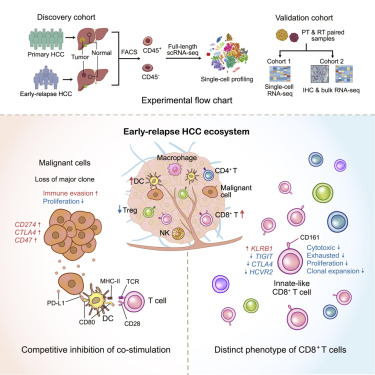
研究表明,这些细胞的富集与较差的预后有关。差异性基因表达和相互作用分析揭示了复发性肿瘤细胞潜在的免疫逃避机制,该机制抑制DC抗原呈递,并招募先天性类似CD8+T细胞。
因此,该研究对HCC生态系统的全面描述为我们提供了与肿瘤复发相关的免疫逃避机制的更深层次的见解。
原始出处:
Yunfan Sun et al. Single-cell landscape of the ecosystem in early-relapse hepatocellular carcinoma. CELL (2020).
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言













#早期复发#
48
#CEL#
49
#Cell#
42
#单细胞测序#现在真火!#樊嘉#院士的研究成果
272
#复旦#
41
早期复发肝癌的单细胞景观
0
该研究对HCC生态系统的全面描述为我们提供了与肿瘤复发相关的免疫逃避机制的更深层次的见解
160
不错
0
肝癌,接下来就要细分了,对于体质好的病人,能否将PD-1类+抗血管新生+放疗等相结合,甚至有必要用TACE进行减负
111