Genes (Basel):前列腺肿瘤组织中MYC DNA甲基化与Gleason评分有关
2021-01-06 AlexYang MedSci原创
越来越多的证据表明前列腺癌中重要的癌症遗传易感区8q24染色体的表观遗传机制存在作用。
越来越多的证据表明前列腺癌中重要的癌症遗传易感区8q24染色体的表观遗传机制存在作用。

最近,有研究人员调查了是否前列腺肿瘤中8q24(从第3个外显子到3'UTR的6个CpG位点)的MYC DNA甲基化是否与肿瘤侵袭性相关(基于Gleason评分,GS),并结合了RNA表达数据研究其功能。研究人员从马里兰大学医学中心获取了50名白种人和50名非裔美国人前列腺癌患者的根治性前列腺切除组织,每组选择同等数量的GS 6和GS 7病例。结果发现,所有6个CpG位点的MYC DNA甲基化在肿瘤中均低于配对的正常前列腺组织(中位数差异:-14.74至-0.20个百分点),他们同样在The Cancer Genome Atlas中观察到附近两个位点的类似结果(p<0.0001)。另外,研究人员在第三个外显子的3个位点中观察到更具侵袭性的肿瘤(GS7)比GS6甲基化水平更低(CpG 212(chr8:128753145),GS 6中位数=89.7%;GS 7的中位数=85.8%;p=9.4×10-4)。MYC DNA甲基化与MYC表达无关,但在多重比较调整后与PRNCR1表达成反比(q=0.04)。
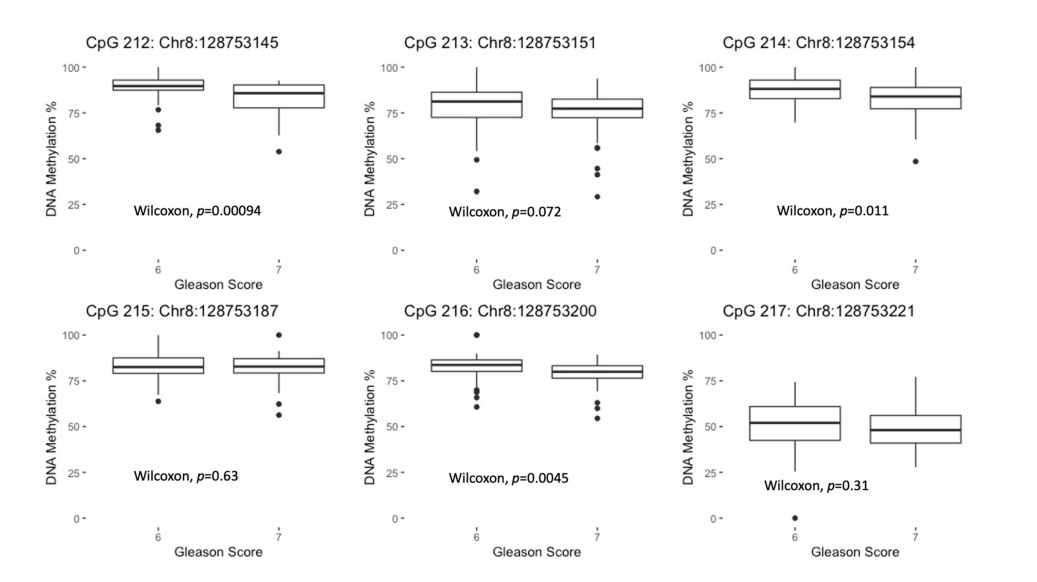
最后,研究人员指出,前列腺肿瘤MYC第3个外显子的低甲基化与侵袭性增加有关。
原始出处:
Kathryn Hughes Barry, Kareshma Mohanty, Patricia A Erickson et al. MYC DNA Methylation in Prostate Tumor Tissue Is Associated with Gleason Score. Genes (Basel). Dec 2020
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言













#Gleason评分#
44
#前列腺肿瘤#
46
#ASO#
47
#Gene#
36
#MYC#
43