JAMA Internal Medicine:每天一杯咖啡,心律失常风险竟降低 3%?!
2021-07-22 “心关注”公众号 “心关注”公众号
戴博士关注到美国加州大学学者昨晚发表在美国医学会杂志子刊《JAMA Internal Medicine》上的文章,该研究评估了喝咖啡(含咖啡因)与异常心律失常风险之间的关系。
喝了咖啡后,心跳可能会加快,有人就说喝咖啡会增加异常心率失常的风险,逻辑上推一下,好像也没毛病。
但真的是这样吗?既往研究并没有给出十分确切的答案。
戴博士关注到美国加州大学学者昨晚发表在美国医学会杂志子刊《JAMA Internal Medicine》上的文章,该研究评估了喝咖啡(含咖啡因)与异常心律失常风险之间的关系。
该项前瞻性队列研究选取了英国生物样本库(U.K. Biobank)中2006年1月至2018年12月的纵向数据,经筛选,最终纳入近39万参与者,平均年龄56岁,女性占比52.3%。
其中,所有参与者每天饮用咖啡的中位杯数为2杯,22.1%的参与者从不饮用咖啡。
在每天饮用咖啡量超过2杯的人群中,年龄相对较高,男性占比更高,吸烟、饮酒的比例更高,外周动脉疾病、癌症的合并率更高,但合并高血压、糖尿病、慢性肾脏疾病的比例相对较低,饮茶人群相对较少。

研究人员将各类型异常心律失常均纳入其中,具体包括房颤或房扑、室上性心动过速、室性心动过速、房性早搏和室性早搏。
平均随访4.5年期间,共16979例参与者发生心律失常,包括12811例房颤,1920例室上性心动过速,909例室性心动过速,97例房性早搏,632例室性早搏,610例未作具体说明的心律失常。
在调整了参与人群的人口统计学特征、共存疾病情况和生活习惯等变量后,发现:在一定范围内,每天每多喝一杯咖啡,心律失常风险降低3%。
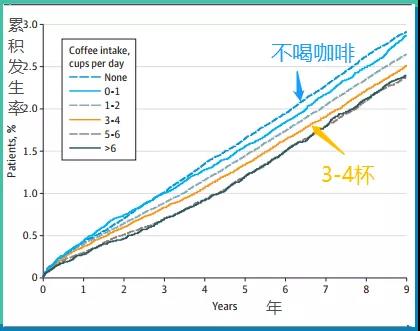
每天饮用不同杯数咖啡人群的心律失常累积发生率
当具体分析各心律失常类型时,注意到喝咖啡与房颤/房扑、室上性心动过速风险的降低程度,与总心律失常风险几乎一致。但喝咖啡与室性心动过速、房性早搏和室性早搏并无关系,不会增加或降低其风险。
另外,即使考虑到可能影响个体代谢咖啡因方式的遗传因素,也未发现二者之间存在关联。
所以,以后要养成喝咖啡的习惯,且多多益善?
这研究对象毕竟是咖啡文化盛行的英国人,谈到咱们国人,笔者认为还是要分情况看待。

对于有喝咖啡习惯的人,如果不存在心脑血管疾病、孕期、骨质疏松等限制,可以根据自己的喜好,每天继续坚持喝咖啡,不用在意一些没有科学依据的所谓“健康”言论。
而对于没有喝咖啡习惯的人,不妨喝点试试,如果不喜欢,也没必要因为看到这项研究提到的益处,而强迫自己喝咖啡。
至于每天的饮用量,虽然加州大学的研究人员发现,每天饮用5-6杯甚至以上时,心律失常的长年累积发生率最低。但如果真的每天大量饮用咖啡,总心脏病风险可是会增加20%以上!切不可为捡芝麻而丢了西瓜。
对咖啡,有点喜欢,适量就好。
原始出处:
Eun-jeong Kim, et al. Coffee Consumption and Incident Tachyarrhythmias Reported Behavior, Mendelian Randomization, and Their Interactions. JAMA Intern Med. Published online July 19, 2021.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言









#CIN#
28
#eRNA#
51
#DIC#
40
#Medicine#
31
#Med#
34
顶刊就是顶刊,谢谢梅斯带来这么高水平的研究报道,我们科里同事经常看梅斯,分享梅斯上的信息
44