J Periodontol:釉质基质衍生物联合非手术疗法治疗中重度牙周炎
2021-09-01 MedSci原创 MedSci原创
牙周炎的治疗旨在阻止进行性骨质和附着丧失,并促使牙周组织再生。发表于J Periodontol的一项多中心研究评估了使用釉质基质衍生物(EMD)作为非手术牙周治疗的辅助手段(测试)与单纯非手术治疗(对
牙周炎的治疗旨在阻止进行性骨质和附着丧失,并促使牙周组织再生。发表于J Periodontol的一项多中心研究评估了使用釉质基质衍生物(EMD)作为非手术牙周治疗的辅助手段(测试)与单纯非手术治疗(对照)的效果。

该项前瞻性、分口、多中心研究纳入51名在同一牙弓内每个对侧象限至少有2个中度至重度牙周炎(PPD=5-8mm)位点的患者,评估使用和不使用EMD的洁治和根面平整术(SRP)。主要结果变量是12个月后临床附着水平(CAL)的变化。次要变量包括探诊深度(PPD)、探诊出血(BoP)、龈缘水平、牙本质过敏,以及转变为不再需要手术治疗的牙周袋的百分比。
结果显示,两种治疗方式的CAL从基线到12个月都有明显变化(P<0.001)(测试组=-2.2±1.5mm,对照组=-2.1±1.3mm),PPD也是如此;组间差异不大。健康位点的PPD(牙周袋<5mm)和转换后的牙周袋(不再需要手术治疗的部位)的百分比方面,观察到明显的差异:测试组79.8% VS. 对照组65.9%。测试部位的牙周病变明显减少(P < 0.05)(测试部位的牙周病为17.8%,对照部位为23.1%)。
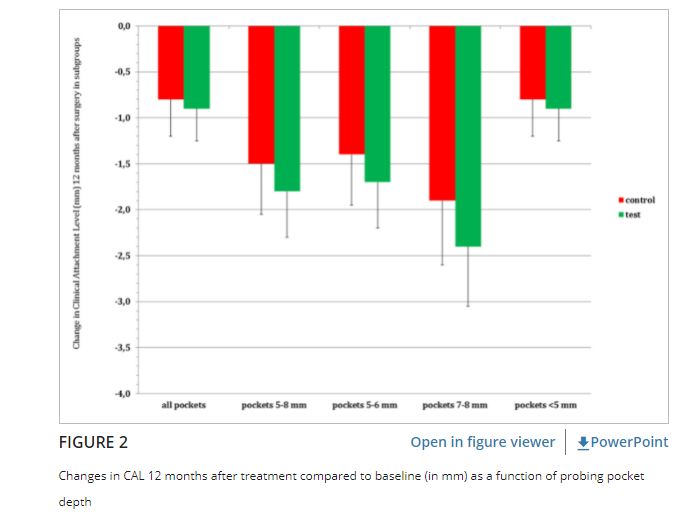
综上,该研究结果表明,测试组和对照组治疗都使CAL和PPD得到了明显的改善。EMD和SRP的辅助使用使整个牙周健康得到了明显的改善,减少了BoP的频率,健康PPD的数量增加。
原始出处:
Rachel A Schallhorn, et al., Application of enamel matrix derivative in conjunction with non-surgical therapy for treatment of moderate to severe periodontitis: A 12-month, randomized prospective, multicenter study. J Periodontol. 2021 May;92(5):619-628. doi: 10.1002/JPER.19-0579. Epub 2020 Oct 21.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#衍生物#
42
#PE#
24
#重度牙周炎#
37
#基质#
36
#牙周#
29