JNNP:多发性硬化症患者的纳比昔莫停药率,一项为期18个月的多中心研究
2020-08-14 MedSci原创 MedSci原创
多发性硬化症(MS)是一种慢性、炎症性和神经变性的中枢神经系统疾病。 痉挛是其最常见的症状之一,大约80%的患者在MS诊断后的第一个十年内出现,并随着时间的推移而恶化。
MS痉挛的治疗方案包括药理学和非药理学策略。抗痉挛药如巴氯芬(口服)、丹曲林、替扎尼丁、加巴喷丁/普雷巴林等,疗效不佳。其他治疗方法,如肉毒杆菌毒素注射和鞘内注射巴氯芬,已证明更有效,但使用有限。 此外,相当多的病人对标准治疗没有足够的反应或有不良反应,特别是长期使用和高剂量。几项研究表明,大约三分之一的患者对抗痉挛疗法的反应不完全。更有相当比例的患者和医生并不完全满足于常见的抗痉挛药物。最近在意大利市场推出的口腔粘膜喷雾剂(Sativex)是MS患者的另一种治疗方案,在常规临床实践中进行的随机临床试验和观察性研究证实,口腔粘膜喷雾剂是治疗耐药性MS痉挛的有效且耐受性良好的选择。但是在6个月的观察期内,有39.5%的患者因疗效降低或不良事件(AE)停药。此外,大多数患者在头三个月内就停止了治疗。
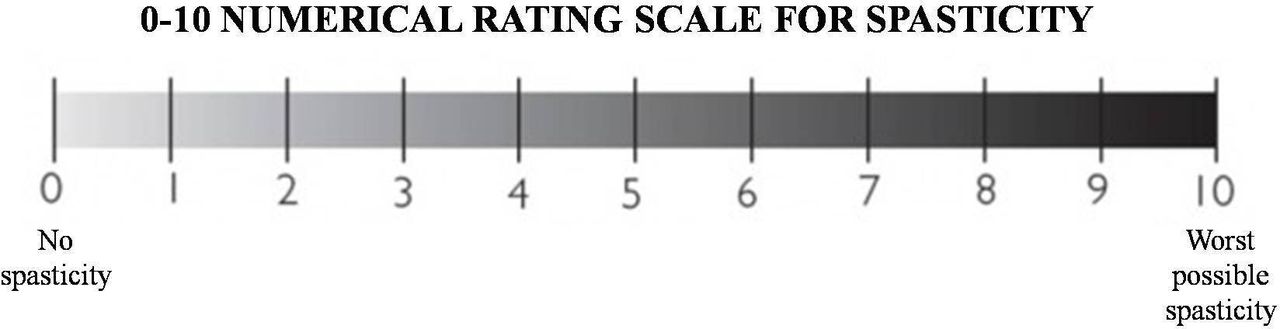
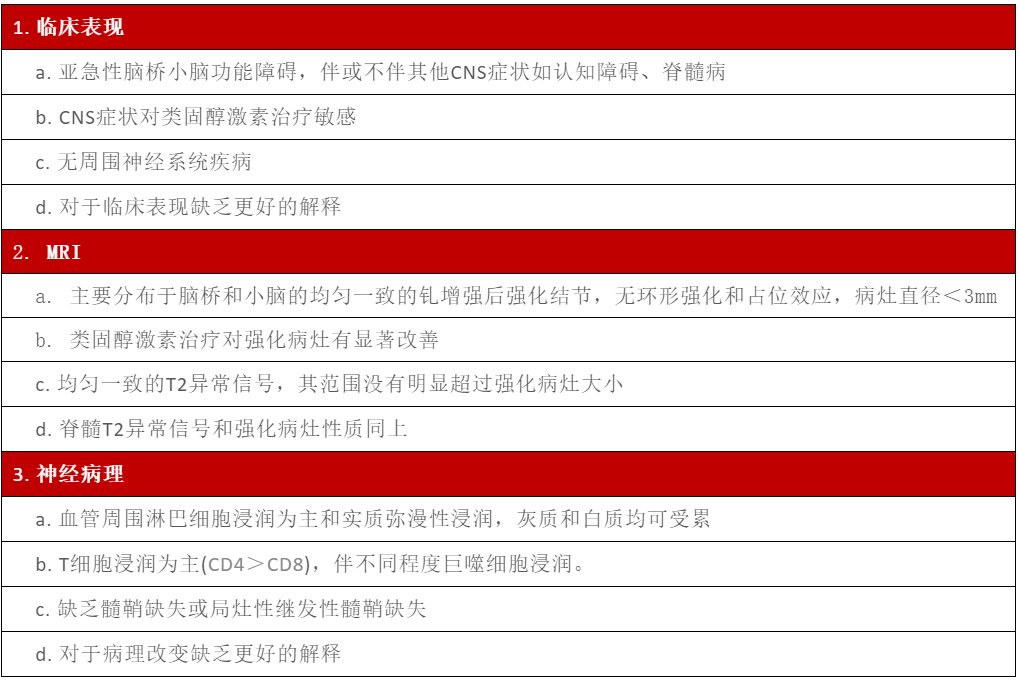
方法:在2015年1月至2018年6月期间,32个MS中心从AIFA Sativex电子注册网站收集了所有患者的数据。所有符合AIFA纳入/排除标准的MS患者均纳入研究队列。分别通过0-10 NRS患者评分量表(0 =否,10 =最大痉挛)和扩展残疾状况量表(EDSS)得出的有关痉挛演变和MS身体残疾的数据。 0-10 NRS是一项在多项研究中用于评估MS痉挛的患者评估指标。特别是,NRS百分比变化(%Δ)在抗痉挛药物的临床试验中被证明是一种有效且可靠的结果指标。人口统计学和临床数据,耐受性,日剂量(每天抽吸量),停药原因和停药日期均通过患者的病历表收集。 此外,还收集了在观察期内发生的不良事件和严重不良事件的数据。 此外,分析了有关NRS值和每个时间点停药的患者百分比的数据。 将所有这些数据手动输入到临时创建的数据库中。

结果:在为期4周的试验期(T1)后,有1502名患者(1845年的81.4%)的NRS改善≥20%(IR),而814名患者(1845的40.2%)≥30%(CRR),平均从基线到T1,NRS得分降低26.9%。在18个月的观察期后,仅考虑IR患者队列,有727名患者(1502名患者的48.3%)停止治疗。总体而言,在观察期内停药的原因是:疗效下降(n = 426,占1502的28.4%),不良事件(n = 256,17.1%),不遵从医嘱(n = 8.0.5%),随访时消失(n = 6.0.4%),患者的自主选择(n = 5,0.3%)或未知(n = 24.16%)。在T2和T3记录了最高的停药率,而从TH4到T5中断THC:CBD的患者比例趋于略有下降。停药的主要原因是分别在T2和T3分别有164和139例患者出现“疗效丧失”。而在T4和T5时,分别有86和47例患者出现AEs是中断THC:CBD治疗的原因。
结论:我们的研究结果证实,在对常规痉挛药没有完全应答的患者中,口腔粘膜喷雾剂(Sativex)是一种有效的选择,是具有良好长期耐受性和安全性的附加疗法。 因此,应该做出特别的努力来改善患者与医生之间的沟通,从而实现对口腔粘膜喷雾剂(Sativex)治疗目标以及实现这些目标的策略的共同看法。
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#多中心研究#
42
#硬化症#
37
#多发性#
0
#多中心#
26
学习了
100
好
104
#停药#
35
好文共享之
100