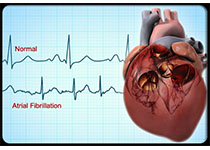
JACC:经胎盘药物治疗胎儿快速心律失常的安全性和可行性研究
2019-09-02 不详 MedSci原创
胎儿快速心律失常的治疗尚没有统一标准。本研究的目的旨在评估经胎盘治疗胎儿室上性心动过速(SVT)和心房扑动(AFL)的有效性和安全性。本研究通过地高辛、索他洛尔和氟卡尼经胎盘对22-37孕周的单胎妊娠的SVT和AFL≥180次/分钟胎儿进行治疗,主要终点事件是胎儿快速心律失常的解决,次要终点事件是胎死、早产和新生儿心律失常。最终,共纳入了来自15个日本医学中心的50名患者,其中短室房SVT胎儿有1
本文系梅斯医学(MedSci)原创编译整理,转载需授权!
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












学习心律失常
67
#可行性#
34
#JACC#
21
#快速心律失常#
26
#ACC#
28
#胎盘#
25