Gut:华西医院最新研究发现,肥胖还喝酒,会让这种致死性急症发生风险更高!
2022-05-30 四五七 MedSci原创
GUT:肥胖是酒精引起重症急性胰腺炎的重要协同因素,大量摄入酒精诱导内脏脂肪分解释放游离脂肪酸是胰腺损伤和多器官功能障碍的关键。
那是我离死亡最近的一刻,在7瓶啤酒下肚后,我开始感到胃胀,虚汗直冒,肚子、后背、腰连着疼,布洛芬都不管用,呕吐到酸水胆汁齐下。
被送到急诊时,我已经虚弱到接近半昏迷状态,抽血化验加CT检查后,我被确诊为重症急性胰腺炎,在ICU住了一个月,前前后后花了10多万,勉强保住了一条命,至今仍感到后怕......
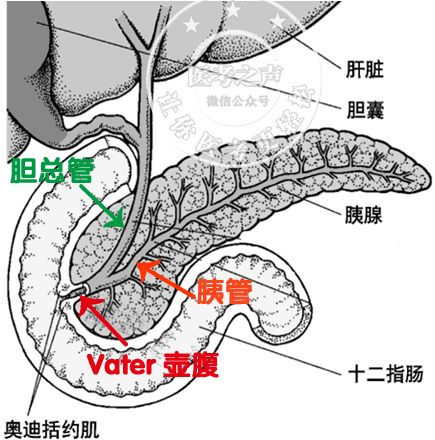
因为大量饮酒而诱发重症急性胰腺炎差点魂断ICU,并不是个例,急性胰腺炎是最常见的消化系统急症,20%的患者会发展成中度至重度急性胰腺炎,在合并多器官障碍的情况下,死亡率高达20%-40%。
酗酒是继胆结石之后急性胰腺炎的主要诱因,酒精摄入量与急性胰腺炎发病率的上升息息相关。
问题是,即使在重度饮酒的人群中,也只有2%-3%的人会出现急性胰腺炎,提示酒精可能不是急性胰腺炎发生的直接原因,在这一过程中还存在其他因素共同发挥作用。
近期,来自四川大学华西医院的夏庆、黄伟及其团队发表在Gut上的一项研究,揭示了肥胖是酒精引起重症急性胰腺炎的重要协同因素,大量摄入酒精诱导内脏脂肪分解释放游离脂肪酸(free fatty acids, FFAs)是胰腺损伤和多器官功能障碍的关键。

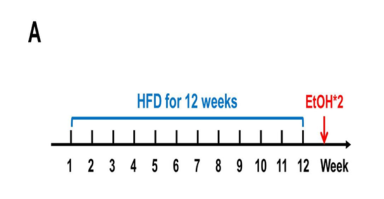
在本实验中,研究对象主要是高脂饮食的肥胖小鼠以及标准饲料喂养的苗条小鼠。
经过12周的高脂/标准饮食后,向小鼠腹腔注射浓度为37.5%乙醇溶液,注射剂量为2g/kg,连续注射2次,时间间隔为1小时,以此来构建重症急性胰腺炎小鼠模型。
肥胖小鼠注射了酒精后的3-6小时内,胰腺组织迅速出现水肿、炎症和坏死,外周血胰酶、胰腺和肺髓过氧化物酶升高,血清IL-6水平上升,多器官损伤指数提高,所有疾病指标在12小时后达到峰值。
然而,和肥胖小鼠不同的是,苗条小鼠注射酒精后,仅仅出现轻微的胰腺水肿,不存在任何重症急性胰腺炎的表现,说明酒精并不能使苗条小鼠出现明显的急性胰腺炎表现。
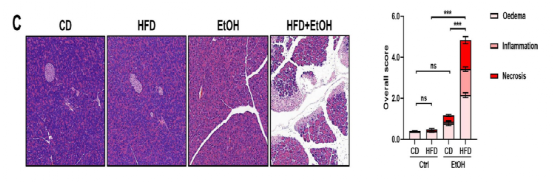
尸检结果显示,酒精注射的肥胖小鼠腹腔、胰腺周围均出现了脂肪皂化(游离脂肪酸与钙离子结合产生皂化反应)。研究人员认为这些游离脂肪酸主要来源于酒精诱导肥胖小鼠内脏脂肪组织的脂肪分解释放。
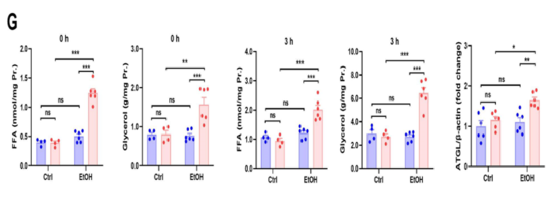
在注射酒精后3小时,肥胖小鼠新鲜分离的附睾脂肪组织中脂肪甘油三酯脂肪酶(adipose triglyceride lipase, ATGL)含量增多,甘油三酯分解产物——游离脂肪酸和甘油释放量大大增加,而苗条小鼠在酒精注射前和注射后,脂肪甘油三酯脂肪酶和游离脂肪酸含量变化并不显著。
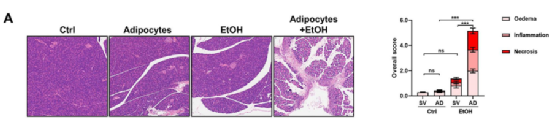
接下来,为了探究这些内脏脂肪组织释放的游离脂肪酸是否是酒精诱导重症急性胰腺炎的关键,研究人员将酒精和来自肥胖小鼠的脂肪细胞一起注射到苗条小鼠腹腔内,成功在苗条小鼠身上复现了肥胖小鼠重症急性胰腺炎的表现,而单独注射酒精或脂肪细胞作都不足以诱导重症急性胰腺炎的发生。
也就是说,只有在酒精和脂肪组织水解释放游离脂肪酸的共同作用情况下,才能产生重症急性胰腺炎。
除此之外,如果提前向肥胖小鼠喂食脂肪甘油三酯脂肪酶抑制剂Atglistatin,抑制脂肪组织脂肪水解释放游离脂肪酸,然后再注射酒精,肥胖小鼠胰腺损伤的情况大大减轻,提前喂食胰腺甘油三酯脂肪酶抑制剂Ortistat则没有这种效果。
再次证明内脏脂肪水解在酒精诱导的重症急性胰腺炎发病过程中发挥重要作用。

总而言之,本研究首次证明了肥胖在酒精诱导急性胰腺炎发生中起着协同作用,内脏脂肪水解释放大量游离脂肪酸也是病情向重症胰腺炎方向发展的扳机。
看来肥胖人群在敞开饮酒前还需掂量掂量自己的将军肚,三思而后行。
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#西医院#
39
#最新#
49
#急症#
45
#华西#
43
#喝酒#
49
#致死性#
29
#研究发现#
27