European Heart Journal:闲暇体力活动,而非工作,与健康益处相关。“体力活动悖论”新证据。
2021-04-16 Dr.Sun Nutrition & Health MedSci原创
体力活动是心血管疾病和全因死亡率的有力预防措施。最近的研究表明,体力活动的潜在健康影响取决于其从事的领域。虽然有大量文件证明闲暇时间体力活动(如体育运动、娱乐和交通)与心血管疾病和全因死亡率呈有益的关
体力活动是心血管疾病和全因死亡率的有力预防措施。最近的研究表明,体力活动的潜在健康影响取决于其从事的领域。虽然有大量文件证明闲暇时间体力活动(如体育运动、娱乐和交通)与心血管疾病和全因死亡率呈有益的关联,但据报道职业性体力活动与改善健康的关联并不一致。
闲暇时间体力活动和职业性体力活动的这种潜在的对比健康效应被称为“体力活动悖论”。对体力活动悖论的解释可能是在闲暇时间和工作期间进行体力活动时非常不同的特征。闲暇时间体力活动通常包括在限定强度水平下的动态运动,足以在短时间内提高心肺适能,有充足的恢复时间。相比之下,工作往往需要静态负荷、单调而笨拙的工作姿势、以及每天几个小时以上的其他非限定活动,而没有足够的恢复时间。
然而,最近的体力活动指南没有在工作和闲暇时间领域之间加以区分。工作是全世界很大一部分成年人从事体力活动的主要领域。目前不知道任何国际或国家体力活动指南将职业性体力活动和闲暇时间体力活动加以区分。如果体力活动悖论成立,这将有助于理解和干预职业性体力活动普遍的个人健康状况不佳的问题。

为了澄清这一悖论,来自丹麦国家工作环境研究中心的研究人员在大型当代哥本哈根一般人群研究中调查了主要不良心血管事件(MACE)和全因死亡风险与职业性体力活动和闲暇时间体力活动的关联,研究结果近日发表在European Heart Journal上。
研究人员在哥本哈根一般人群研究中对104046名年龄在20-100岁之间的男性和女性进行了研究,2003-2014年进行了基线测量,随访中位数10年。闲暇和职业性体力活动都根据自我报告分为四类应答。研究人员观察到7913例(7.6%)MACE和9846例(9.5%)全因死亡。与闲暇时间低体力活动相比,MACE的多变量调整(生活方式、健康、生活条件和社会经济因素)危险比在中体力活动为0.86(0.78-0.96)、高体力活动为0.77(0.69-0.86),极高体力活动为0.85(0.73-0.98);较高职业性体力活动的相应值分别为1.04(0.95-1.14)、1.15(1.04–1.28)和1.35(1.14-1.59)。就全因死亡率而言,较高闲暇时间体力活动的相应危险比为0.74(0.68-0.81)、0.59(0.54–0.64)和0.60(0.52–0.0.69),较高职业性体力活动分别为1.06(0.96-1.16)、1.13(1.01–1.27)和1.27(1.05-1.54)。排除在随访前5年内死亡的个体后,在生活方式、健康、生活条件和社会经济因素各分层中也发现了类似的结果。两种领域的体力活动水平对MACE(P = 0.40)或全因死亡率(P = 0.31)的风险没有相互作用。
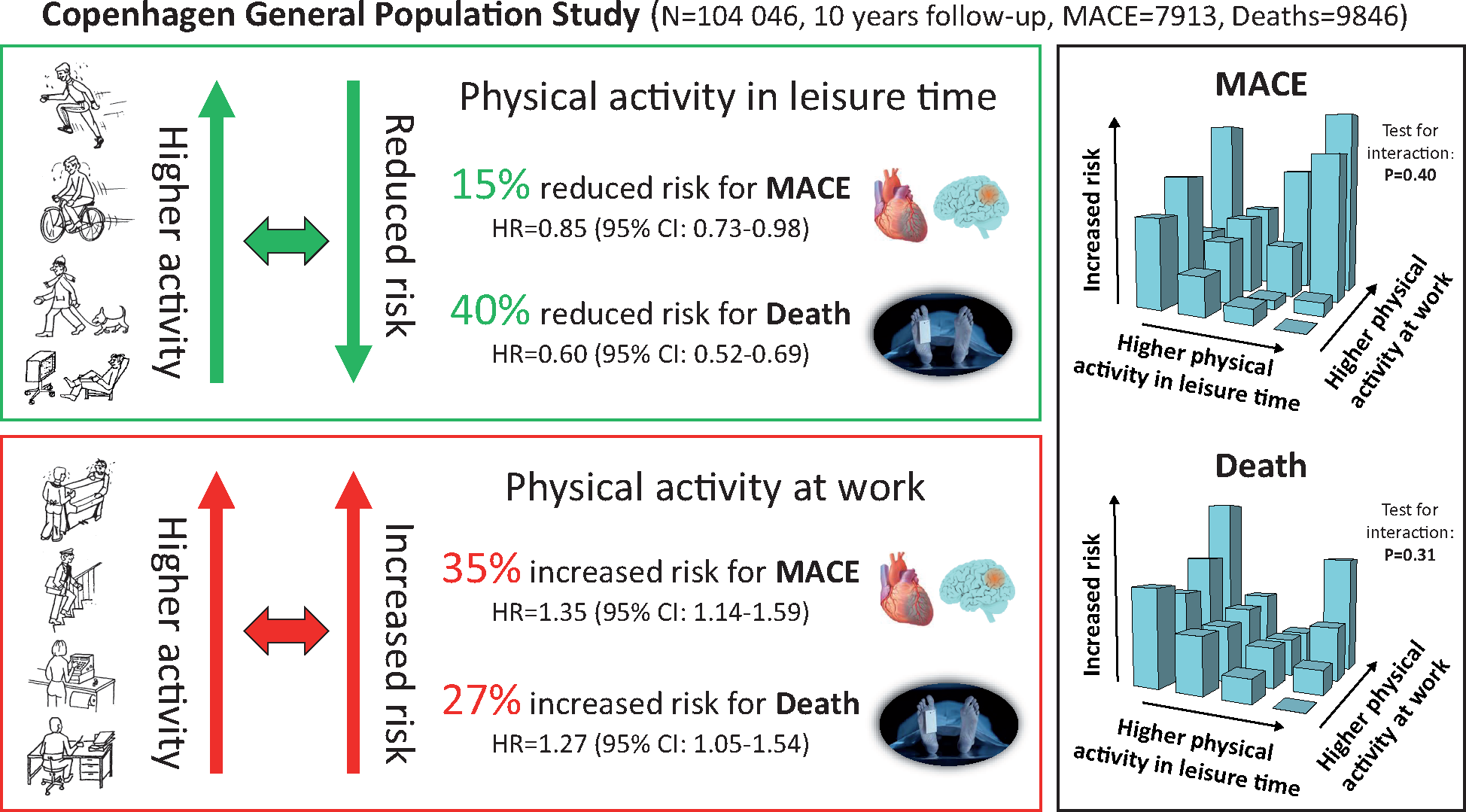
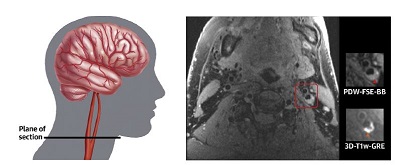
在哥本哈根一般人群研究中,主要不良心血管事件(MACE)和全因死亡率的风险作为个人不同类别闲暇时间体力活动和职业性体力活动的函数。

闲暇时间体力活动和职业性体力活动与主要不良心血管事件和全因死亡率风险的关联。
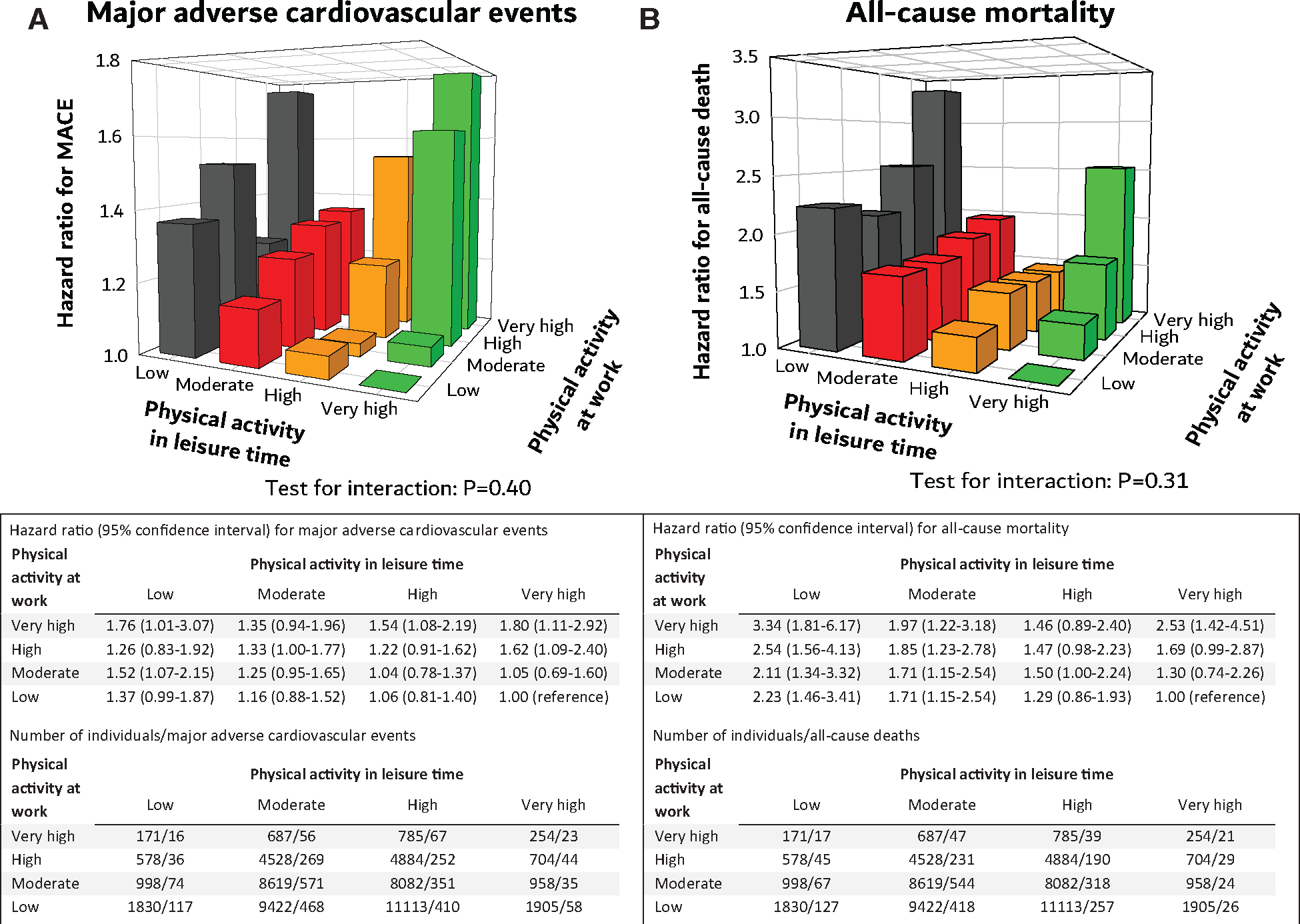
对于(A)主要不良心血管事件和(B)全因死亡率风险,四个闲暇时间体力活动类别和四个职业性体力活动类别之间相互作用。

一级较高的闲暇时间体力活动(A)或职业性体力活动(B)与整体和分层后主要不良心血管事件发生风险的关联。

一级较高的闲暇时间体力活动(A)或职业性体力活动(B)与整体和分层后全因死亡率风险的关联。
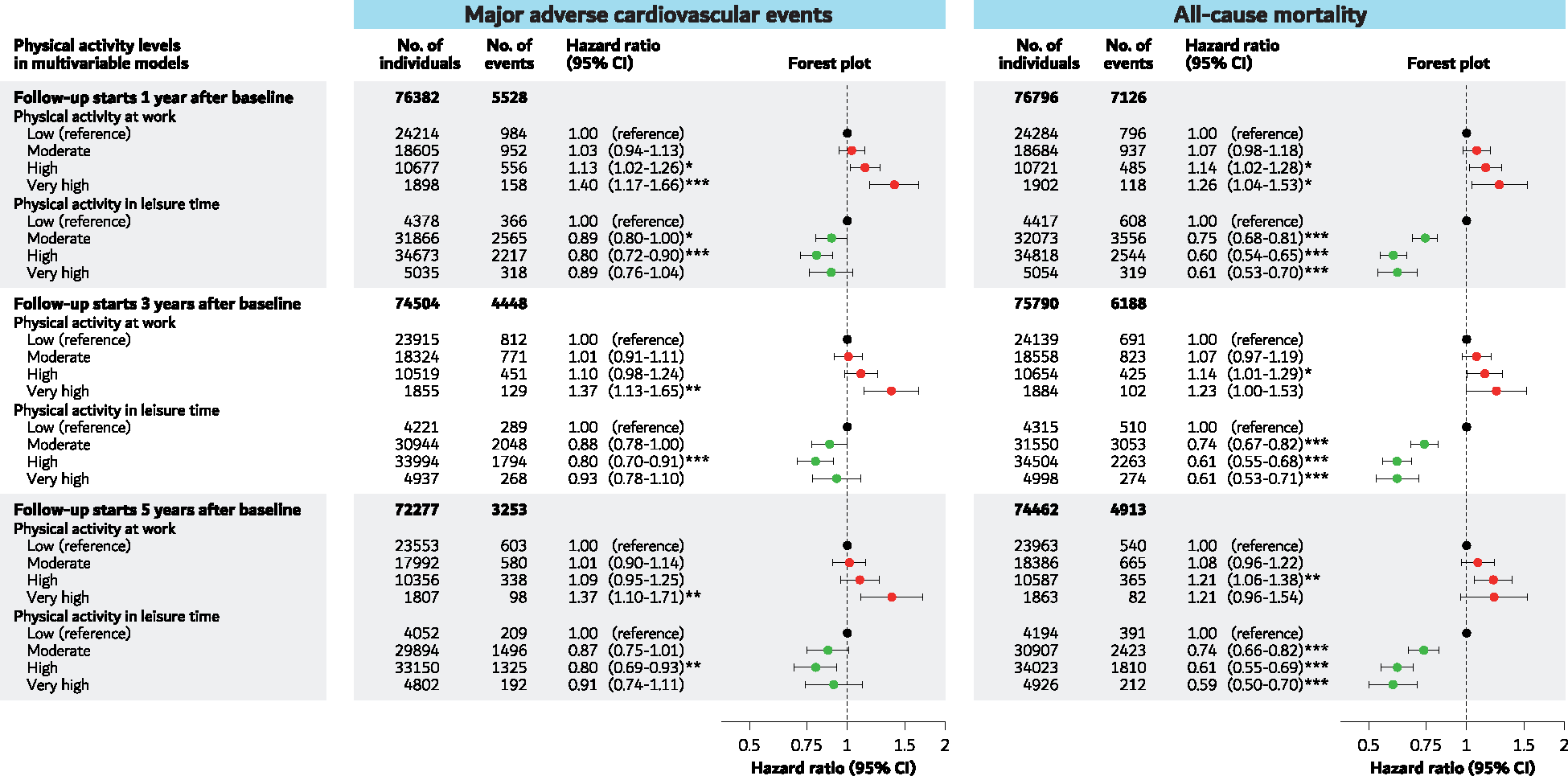
闲暇时间体力活动和职业性体力活动与主要不良心血管事件和全因死亡率风险的关联,分别在基线后1年、3年和5年开始随访。
总之,研究发现,较高的闲暇时间体力活动与主要不良心血管事件(MACE)风险和全因死亡率降低有关,而较高的职业性体力活动则与风险增加有关,彼此独立。这两种类型的体力活动对MACE和全因死亡率风险的独立关联的这一最新证据支持了体力活动悖论。那些撰写与体力活动有关的心血管疾病预防指南的人可以将这些发现纳入参考。
原始出处:
Andreas Holtermann, Peter Schnohr et al. The physical activity paradox in cardiovascular disease and all-cause mortality: the contemporary Copenhagen General Population Study with 104 046 adults. Eur Heart J. 2021 Apr 14;42(15):1499-1511. doi: 10.1093/eurheartj/ehab087.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











#PE#
32
#ART#
31
#HEART#
40
已读,真是受益匪浅呀!
79
想退休了
69
学习了
64
看来确实需要劳逸结合!
52