Sci Rep:尿液中的miRNA谱可鉴定梗阻引起的膀胱功能障碍
2021-05-18 AlexYang MedSci原创
下尿路功能障碍(LUTD)患者有一系列的症状,如日间和夜间排尿频率增加、尿急、尿失禁、尿流缓慢、犹豫不决和排不净。连续的上厕所、睡眠周期的紊乱、尿失禁和频繁的尿路感染强烈地影响了他们的生活质量,身体及
下尿路功能障碍(LUTD)患者有一系列的症状,如日间和夜间排尿频率增加、尿急、尿失禁、尿流缓慢、犹豫不决和排不净。连续的上厕所、睡眠周期的紊乱、尿失禁和频繁的尿路感染强烈地影响了他们的生活质量,身体及情感的健康。

据估计,全世界有45%的人口受到至少一种下尿路(LUT)症状的影响,这些症状可由各种病症引起,包括膀胱出口梗阻(BOO)、膀胱疼痛综合征、膀胱过度活动综合征和神经系统疾病(包括脊髓损伤、帕金森氏病和多发性硬化症)。LUTD能够引起巨大的社会经济负担:在美国,膀胱过度活动症(OAB)患者的医疗费用是没有过度活动症类似患者的2.5倍以上。这也是将老年人转移到养老院的主要原因之一,进一步增加了医疗费用,损害了他们的生活标准。随着人口的老龄化,多因素性LUTD的发病率也在不断增加。
尿急、尿频和排不净是良性前列腺梗阻(BLUTD)和神经源性(NLUTD)下尿路功能障碍之间经常共有的症状。之前研究人员利用膀胱活检,提出了一个针对膀胱不同功能表型的miRNA生物标志物。尿液是循环miRNA的良好来源,性别和年龄匹配的对照组对于尿液代谢物的比较很重要。
研究人员在两组健康受试者(平均年龄分别为32岁和57岁)中发现,各年龄组尿液中的总蛋白和RNA含量非常相似,但年轻健康男性受试者的分泌细胞外囊泡(uEVs)的数量和几种miRNA的含量更高。另外,尿液收集的时间对这些参数影响不大。研究人员还评估了尿液miRNAs对膀胱出口梗阻(BOO)的非侵入性诊断的适用性。结果发现,三个尿液miRNA(miR-10a-5p、miR-301b-3p和miR-363-3p)可以区分对照组和LUTD(BLUTD和NLUTD)患者。
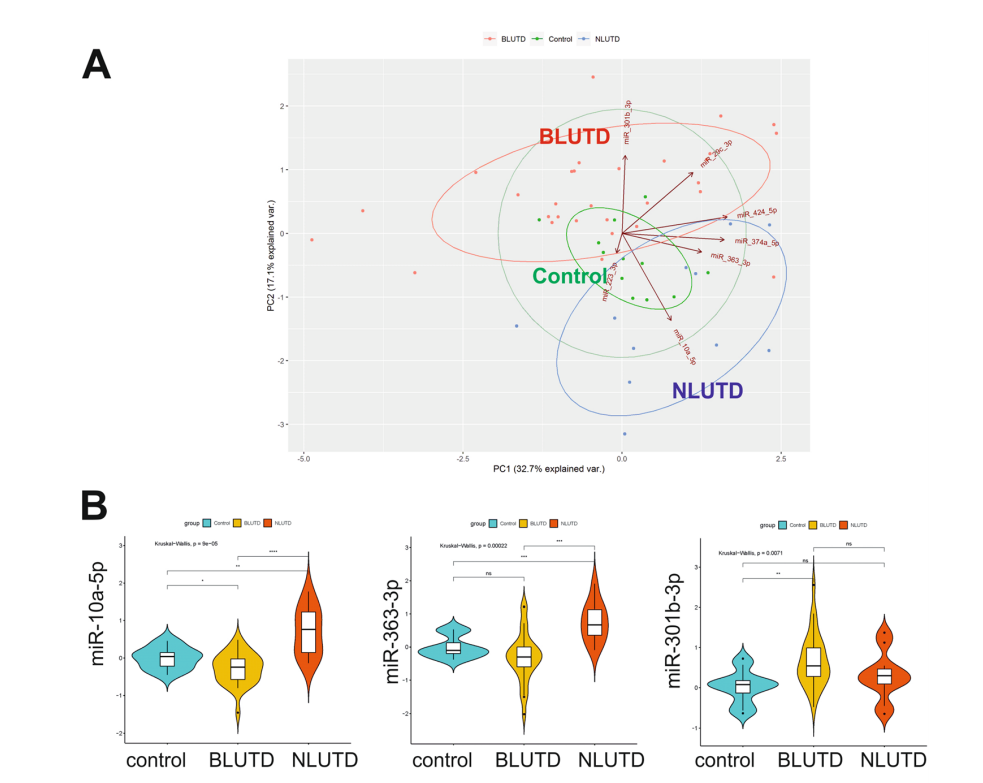
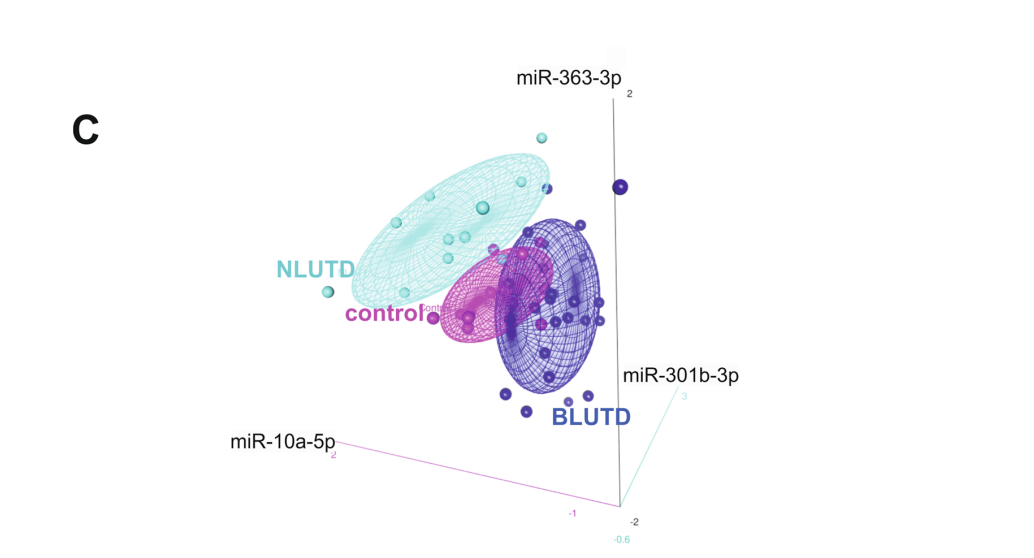
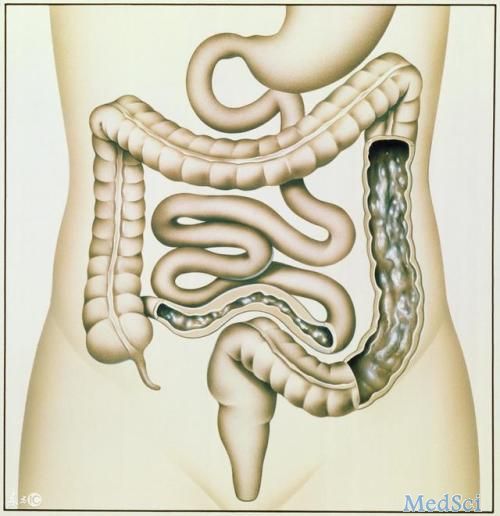
膀胱梗阻引起的LUTD中尿液生物标记miRNAs的鉴定
他们提出的代表性miRNAs可以用于进一步的探索,从而开发一个非侵入性的BOO诊断测试。另外,他们观察到的尿液miRNA含量与年龄有关,因此,选择适当的、年龄匹配的对照也是很重要的。
原始出处:
Michelle von Siebenthal, Mustafa Besic, Ali Hashemi Gheinani et al. Urinary miRNA profiles discriminate between obstruction-induced bladder dysfunction and healthy controls. Sci Rep. May 2021
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











#膀胱功能#
30
#miR#
27
#miRNA#
38
#功能障碍#
34
#尿液#
50
很好
61