Eur J Cancer:卡培他滨辅助治疗对乳腺癌患者生存预后的影响
2022-03-21 xiaozeng MedSci原创
卡培他滨可改善三阴性乳腺癌患者的无病生存预后和总生存预后,加入系统治疗时还可改善所有早期乳腺癌患者的无病生存预后和总生存预后
虽然在随机试验中有大量早期乳腺癌(EBC)患者接受过卡培他滨治疗,但尚未对接受卡培他滨治疗的早期乳腺癌个体患者数据进行过荟萃分析。近日,《Eur J Cancer》期刊上发表了一项研究,评估了卡培他滨在早期乳腺癌患者中的疗效和毒性。
研究人员根据以下标准:早期乳腺癌患者采用卡培他滨作为辅助或新辅助治疗,超过100位患者的多中心随机试验,招募已完成、预后可评估,在clinicaltrials和pubmed数据库中检索了符合要求的临床试验。主要终点是卡培他滨对无病生存期(DFS)的影响,次要终点是分析远期DFS(DDFS)、总生存期(OS)、病理完全缓解率和卡培他滨相关毒性与治疗效果的相互作用。
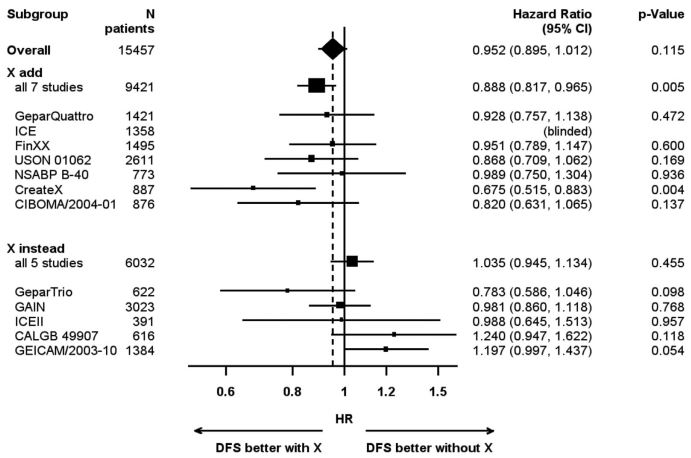
加用或换用卡培他滨对DFS的影响
筛查到13项符合标准的试验,共包含15993位患者。对所有纳入的患者进行Cox回归分析显示,与不加用卡培他滨的治疗相比,加用卡培他滨并未能显著改善早期乳腺癌的DFS(HR 0.952; 95% CI 0.895-1.012; P=0.115)。在使用卡培他滨代替其他药物的亚组研究中,加用卡培他滨也无明显有益作用(HR 1.035; 95% CI 0.945-1.134; P=0.455)。
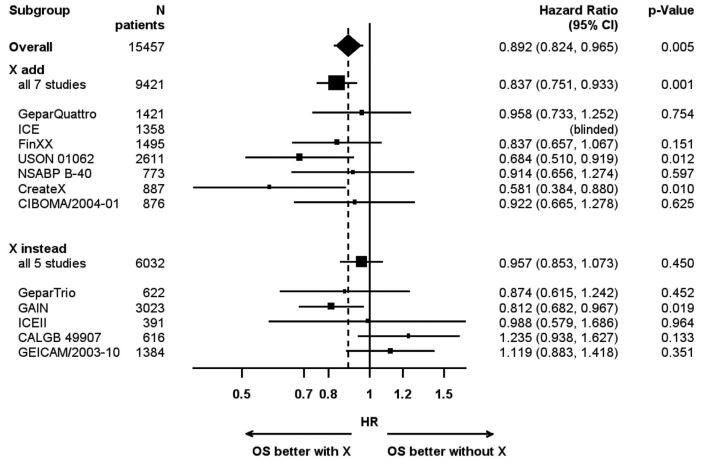
加用或换用卡培他滨对OS的影响
但是,卡培他滨联合标准全身治疗可改善DFS(HR 0.888; 95% CI 0.817-0.965; P=0.005)。在整个研究队列和加用卡培他滨的亚集中,总生存期均有所提高(HR 0.892; 95% CI 0.824-0.965, P=0.005;HR 0.837; 95% CI 0.751-0.933, P=0.001)。亚组分析显示,无论是在DFS方面,还是在OS方面,三阴性乳腺癌 (TNBC) 患者均可卡培他滨总体以及加入其他全身治疗中获益。
综上所述,卡培他滨可改善三阴性乳腺癌患者的无病生存预后和总生存预后,加入系统治疗时还可改善所有早期乳腺癌患者的无病生存预后和总生存预后。
原始出处:
van Mackelenbergh Marion T,Seither Fenja,Mobus Volker et al. Effects of capecitabine as part of neo-/adjuvant chemotherapy - A meta-analysis of individual breast cancer patient data from 13 randomised trials including 15,993 patients.[J] .Eur J Cancer, 2022, 166: 185-201. https://doi.org/10.1016/j.ejca.2022.02.003
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#患者生存#
46
#生存预后#
50
#卡培他滨#
49
#乳腺癌患者#
46