J Clin Periodontol:局部应用釉基质蛋白预防牙周再生术后的急性全身性炎症
2020-05-31 网络 网络
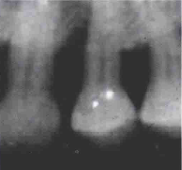
本实验旨在研究健康人使用釉基质蛋白(EMD)辅助手术治疗牙周骨吸收(IBD)的急相期反应。
本实验旨在研究健康人使用釉基质蛋白(EMD)辅助手术治疗牙周骨吸收(IBD)的急相期反应。
研究纳入38个牙周炎患者(每个患者有1个IDB),随机分为2组,有/无EMD辅助微创牙周手术。记录术前和术后6个月时的牙周参数。在术前,术后1天、7天和180天采集血液样本。
结果发现,术后24小时,EMD+MIS组的C-反应蛋白(CRP;p<.01)较低,没有炎症干扰。相反,MIS组在24小时(p<.05)时产生急性炎症反应,第7天回归到其基础值。术后6个月,EMD+MIS组没有BOP或PPD≥5mm的病例更多(p<.05),术后牙龈退缩较少(p<.05)。
EMD辅助手术治疗可以使术后24小时的血清CRP水平降低,改善急性炎症反应和临床牙周参数。因此,EMD可能具有全身性抗炎作用。
原文出处:
FilippoGraziani, Local application of enamel matrix derivative prevents acute systemic inflammation after periodontal regenerative surgery: A randomized controlled clinical trial,Journal of clinical periodontology, 2020 June,doi.org/10.1111/jcpe.13270
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言













#釉基质蛋白#
30
#PE#
37
#基质#
31
#局部#
36
#牙周#
41
#牙周再生#
31