JAMA Netw open:转移性肾细胞癌患者“免疫-肿瘤联合治疗”后的影像学反应
2022-06-26 liangying MedSci原创
这项研究发现,与IOIO治疗相比,IOVE治疗与客观成像反应的几率显著增加相关。肺转移、接受细胞减灭性肾切除术和良好的IMDC风险与出现客观影像学反应的几率增加相关。
转移性肾细胞癌(mRCC)患者的总体生存率(OS)的改善是通过使用针对免疫检查点阻断(ICB)和血管内皮生长因子(VEGF)受体的药物的联合治疗方法实现的。患者和医生有许多一线免疫肿瘤学(IO)治疗选择,包括使用伊普利单抗nivolumab(IOIO)的双重ICB治疗或使用VEGF受体抑制剂(IOVE;包括阿维单抗、阿维替尼pembrolizumab、卡博扎尼nivolumab和伦伐替尼pembrolizumab)的ICB治疗联合治疗。然而,大多数患者最终会对这些疗法产生耐药性。
在转移性肾细胞癌(mRCC)患者中,一线免疫-肿瘤(IO)联合治疗与医生评估的客观影像学反应之间的关联仍未明确。本研究的目的是比较mRCC患者一线IO联合伊普利单抗nivolumab(IOIO)治疗与经批准IO联合VEGF抑制剂(IOVE)治疗的客观影像学反应(即完全或部分反应)的可能性。

这项多中心国际队列研究嵌套在常规临床实践中。国际转移性肾细胞癌数据库联盟(IMDC)的数据集用于确定2013年5月30日至2021年9月9日期间接受IO联合治疗的连续mRCC患者。共有899名经组织学证实诊断为mRCC的患者接受一线IOVE或IOIO方案治疗,并有可评估的反应。
研究的主要结果是医生根据接受的一线IO联合治疗类型评估客观影像反应的差异。次要结果包括确定与客观影像反应呈正相关的基线特征,以及客观影像反应与总生存率的相关性。
结果显示,在1085名接受一线IO联合治疗的mRCC患者中,899名患者有可评估的反应。共有794名患者掌握IMDC风险分类信息;其中,127例(16.0%)有良好风险,442例(55.7%)有中等风险,225例(28.3%)有较差风险。在所有参与者中,就最佳总体反应而言,37名患者(4.1%)完全缓解,344名患者(38.3%)部分缓解,315名患者(35.0%)病情稳定,203名患者(22.6%)病情进展。相应的中位总生存期在完全缓解患者、部分缓解患者、稳定患者和进展患者中分别为55.9个月、48.1个月和13.0个月。与IOIO治疗相比,IOVE治疗与获得反应的可能性增加独立相关。肺转移、接受细胞减灭性肾切除术和良好的IMDC风险与反应可能性增加独立相关。
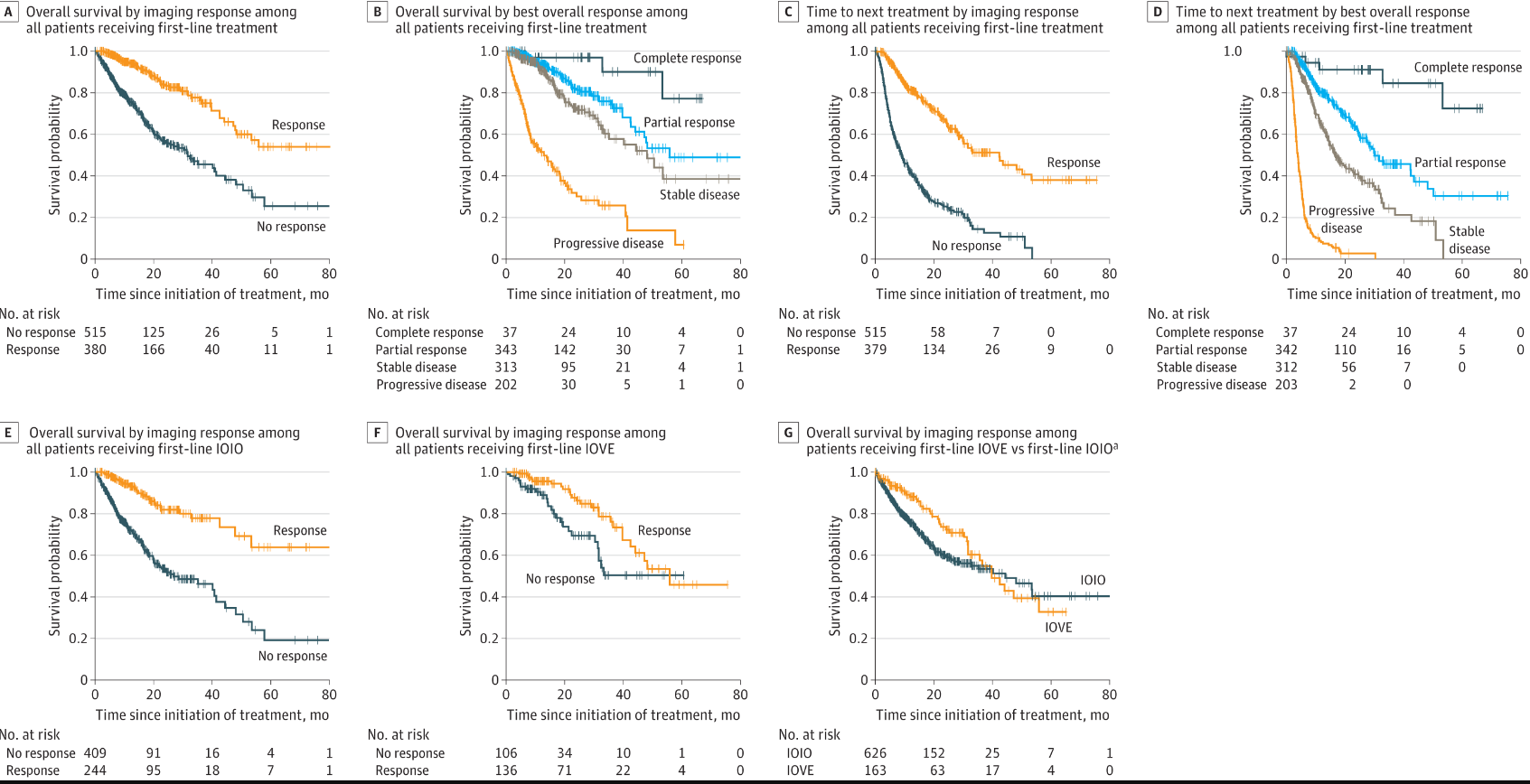
Kaplan-Meier总生存率和下一次治疗的时间
总之,这项研究发现,与IOIO治疗相比,IOVE治疗与客观成像反应的几率显著增加相关。肺转移、接受细胞减灭性肾切除术和良好的IMDC风险与出现客观影像学反应的几率增加相关。这些发现可能有助于指导临床上的治疗选择,尤其是在与高容量多部位转移性疾病相关的临床环境中,获得客观的影像学反应非常重要。
参考文献:Navani V, Ernst M, Wells JC, et al. Imaging Response to Contemporary Immuno-oncology Combination Therapies in Patients With Metastatic Renal Cell Carcinoma. JAMA Netw Open. 2022;5(6):e2216379. doi:10.1001/jamanetworkopen.2022.16379
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言













#NET#
53
#PE#
22
#细胞癌#
31
#联合治疗#
34
#转移性#
40
#转移性肾细胞癌#
34
JAMA上文章都是顶级的,谢谢梅斯及时上新
22