JAMA:宣武医院焦力群教授团队证实症状性颅内动脉狭窄血管内治疗未见获益(CASSISS研究)
2022-08-10 CASSISS研究组 卒中视界
梅斯点评:JAMA几乎同时发表了两篇中国学者主导的、神经内科的研究成果,而且均为阴性。RESCUE BT研究未能发现替罗非班在大血管闭塞性卒中患者中获益,见:JAMA:血管内治疗前经静脉使用替罗非班并
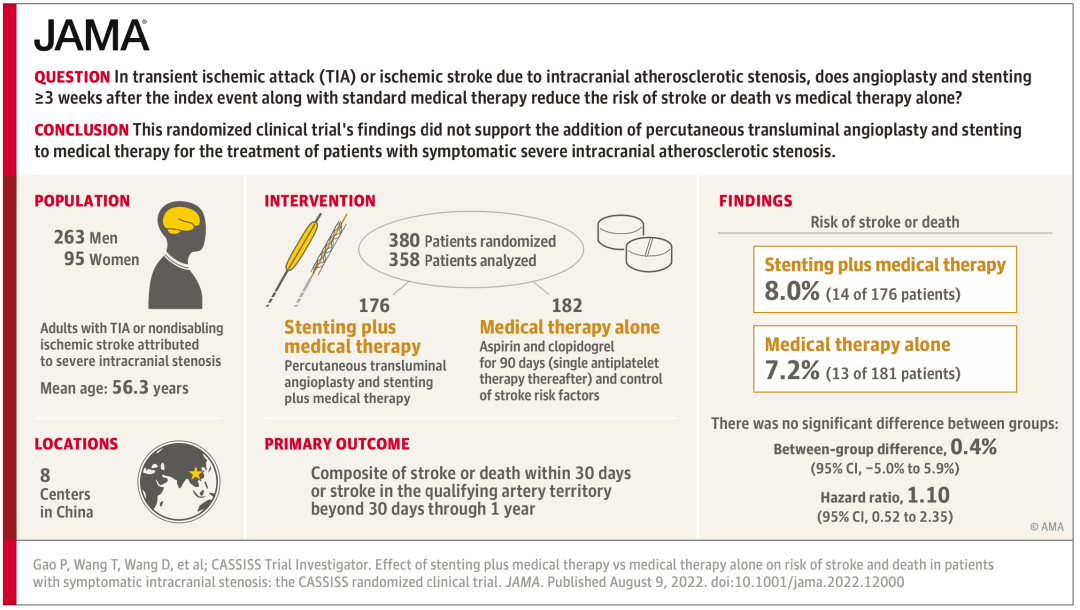
梅斯点评:JAMA几乎同时发表了两篇中国学者主导的、神经内科的研究成果,而且均为阴性。RESCUE BT研究未能发现替罗非班在大血管闭塞性卒中患者中获益,见:JAMA:血管内治疗前经静脉使用替罗非班并不显著改善大血管闭塞性卒中患者的临床结局(RESCUE BT研究)。这篇CASSISS研究也未能发现对症状性颅内动脉狭窄的血管内治疗获益,结论有些令人意外,但是也在情理之中,任何一项技术的探索,都是曲折的过程。不过两项研究结果的发表,也体现了中国在神经病学领域的逐步打造出科研的高地!自从2015年王拥军教授的CHANCE研究在NEJM上发表以后,神经病学领域的学者越来越不惧怕顶级刊物了!期刊将来有更多重磅的成果发表! 2022年8月10日凌晨,由首都医科大学宣武医院神经外科焦力群教授团队领衔,联合中国8家医院共同开展的多中心、随机对照临床试验——CASSISS研究结果在线发表在国际顶级医学期刊《JAMA》。历时10年的CASSISS研究在国际上为颅内动脉狭窄的血管内治疗提供了新的医学证据。CASSISS研究对比了支架联合药物治疗vs单纯药物治疗对症状性颅内动脉狭窄患者卒中和死亡的影响。研究结果显示,对于症状性、重度颅内动脉狭窄的患者,支架联合药物治疗在预防卒中或死亡方面,与单纯药物治疗相当。 背景 脑卒中是我国首位致死病因。颅内动脉粥样硬化狭窄是亚洲人群高发的缺血性脑卒中病因,比例可高达46.6%。而在西方国家,该比例仅为10%-15%。因此,颅内动脉粥样硬化狭窄是中国缺血性卒中最常见的病因之一,对我们脑卒中的防治工作带来了巨大挑战。 介入支架置入术等血管内治疗一直被视为颅内动脉粥样硬化狭窄有潜力的治疗手段。美国的SAMMPRIS和VISSIT研究是全球仅有的两项对比支架与单纯药物治疗的多中心随机对照研究,均主要在西方人群中完成。其结果显示,支架治疗具有较高并发症,比单纯药物治疗更差;但对这两个研究,学术界历来有很多质疑。 近年来,国内外多个前瞻性登记研究、真实世界研究均显示颅内动脉支架还是安全的,并发症风险仅为2.0%-4.3%,与SAMMPRIS研究的14.7%形成鲜明的反差。因此,颅内动脉粥样硬化狭窄的治疗策略尚存争议。 鉴于SAMMPRIS研究以美国白种人为主体,以及其自身试验设计的缺陷,时代迫切需要中国的数据,借助中国医生努力和贡献,来验证血管内治疗在国人数据的安全性和有效性。因此,在“十二五”国家科技支撑计划支持下,CASSISS研究应时代而生。 CASSISS研究(中国血管成形及支架置入术治疗症状性重度颅内动脉狭窄:一项多中心、随机对照临床试验)是目前全球第三个、中国和亚洲第一个多中心随机对照临床试验,由首都医科大学宣武医院、国家神经疾病医学中心焦力群教授团队牵头,联合北京医院王大明教授、哈尔滨医科大学附属第一医院史怀璋教授、战略支援部队特色医学中心蔡艺灵教授、山东大学齐鲁医院吴伟教授、河南省人民医院李天晓教授、空军军医大学唐都医院赵振伟教授、广州医科大学附属第二医院何伟文教授团队,共同完成,对患者选择标准、手术时机、医学中心容量等进行了优化,评估支架和单纯药物治疗对症状性、重度颅内动脉粥样硬化性狭窄患者的卒中或死亡的防治效果。经全体研究者历经近十年的齐心协作和不懈努力,该研究成果最终在国际顶级医学期刊《JAMA》上公开发表。 方法 针对SAMMPRIS研究的设计缺陷,CASSISS研究提出两方面的重要改进: 1 选择更有经验的医生和更严格的筛选患者,降低30天并发症(安全性); 2 延长随访时间至3年,观察血管内治疗对颅内动脉狭窄的长期保护性(有效性)。 因此,CASSISS研究其设计目的在于重新评估血管内治疗对颅内动脉狭窄的安全性和有效性,为国际上颅内动脉狭窄治疗提供国人证据。

CASSISS研究创新性地设置了两阶段试验:一期先导性试验和二期随机对照试验。
先导性试验阶段:
为前瞻性、单臂的观察性研究。2013年7月-2014年3月,依据后续随机对照试验的纳入排除标准,连续纳入100名患者进行支架治疗,评估围术期手术风险,确保受试者安全性和参与中心资质,验证后续RCT试验的可操作性。结果显示,该组患者支架术后的30天卒中或死亡比例为2.0%,远低于SAMMPRIS和VISSIT研究结果。先导性试验验证了后续RCT试验的可操作性,并通过该期研究将研究中心从13家压缩到更有资质的8家。
随机对照试验阶段:
为多中心、开放标签、盲法评估的随机对照临床试验。2014年3月至2016年11月,从8家医学中心,共纳入了380例缺血事件发作超过3周,表现为TIA或非致残、非穿支区缺血性卒中,狭窄程度为重度(70%-99%)的颅内动脉粥样硬化性狭窄患者。按照1:1的比例,随机分为支架联合药物治疗和单纯药物治疗两组。主要结局为30天内卒中或死亡及30天至1年的责任血管区域卒中,次要结局包括2年或3年的责任血管区域卒中或死亡等。随访期为3年,2019年11月10日结束最后一名患者的随访。
结果
在380例患者中,最终确认358 例患者符合入组条件并完成了试验,其中支架组为176例,药物组为181例。
主要结局显示:支架联合药物治疗与单纯药物治疗相比,无显著的统计学差异(8.0% [14/176] vs. 7.2% [13/181];风险比:1.10, 95%CI 0.52-2.35;P=0.82)。在5个次要结局中,均未显示出显著的统计学差异。例如,3年责任血管区域卒中(11.3% [19/168] vs. 11.2% [19/170];风险比 1.00,95%CI 0.53-1.90;P=1.00)。两组的3年死亡率分别为 4.4% [7/160] 和 1.3% [2/159](风险比,3.75 [95% CI 0.77-18.13];P =0.08)。
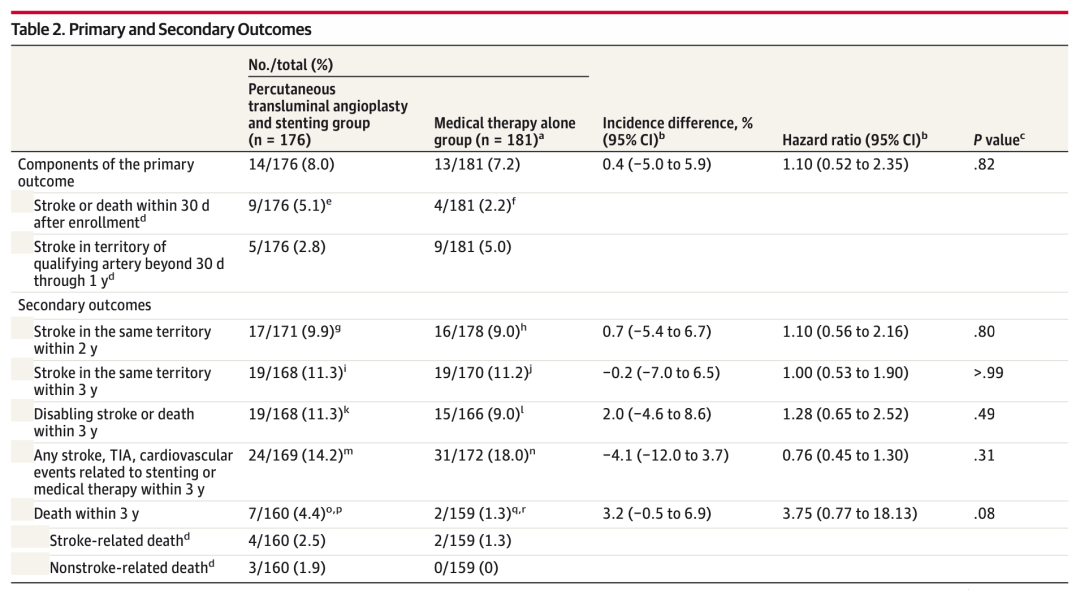
主要和次要结局

主要结局的K-M曲线
结论
对于症状性颅内动脉粥样硬化性狭窄导致的TIA或缺血性脑卒中患者,在药物治疗的基础上联合支架治疗与单纯的药物治疗相比,30天内卒中或死亡的风险以及30天至1年内责任血管区域卒中的风险无显著差异。(CASSISS研究由“十二五”国家科技支撑计划支持,项目编号为2011BAI08B04, ClinicalTrials.gov注册号为NCT01763320)
CASSISS研究以高质量的研究数据和高级别的证据级别,解决了该领域长达二十年的争议,或将成为本领域临床指南的“收官之作”,重要的结论在于:
1 经验丰富的中国医生可以获得明显优于美国研究的安全性,有效性不劣于药物治疗;
2 在现行颅内动脉粥样硬化性狭窄的诊断评估体系下,介入支架治疗相比于单纯药物治疗,患者并没有额外获益。
CASSISS研究也为未来颅内动脉粥样硬化性狭窄的研究方向提供了重要启示。未来的研究会集中于疾病诊断评估的理念和技术革新,以及介入治疗器械和技术的进步。
共同一作

高鹏,副主任医师,医学博士。
神经外科副主任医师,医学博士,北京市科技新星,国家教育部公派留学生。
北京医学会介入医学分会青年委员会副主任委员,北京医学会介入医学分会委员会神经介入学组委员兼秘书,中国医师协会神经介入专业委员会青年委员会委员。
一直致力于缺血性脑血管疾病的临床诊治工作。2007年-2009年,曾在美国加州大学旧金山分校脑血管病研究所学习。以第一作者身份发表SCI论文12篇,参编参议著作各一部。主持国家自然科学基金青年基金和北京市科委科技新星计划各一项。参与国家“十二五”科技支撑计划课题《缺血性脑血管病脑血运重建微创技术体系研究》和“十三五”国家重点科技支撑计划《数字化脑血流储备功能诊断评估技术及其应用研究》。

王韬,主治医师,医学博士。
2017年毕业于北京协和医学院(清华大学医学部)临床医学八年制。致力于颅内动脉狭窄、颈动脉狭窄和烟雾病等缺血性脑血管病的外科及介入诊疗。迄今以第一作者或共同第一作者发表SCI论文20篇,中文核心期刊论文1篇。参编书籍2部。参与“十三五”国家重点研发计划、北京市科委等省部级课题,主持北京市医管中心培育计划等3项课题。对临床背景下的数据挖掘和信息分析有较深入的了解,擅长临床研究设计和系统评价方法。成功注册多项Cochrane系统评价,对颅内动脉狭窄和颈动脉狭窄的诊断、评估及治疗方式进行了研究。

王大明,主任医师,教授,博士生导师,全国政协委员。
现任北京医院神经外科首席专家。兼任中华神经外科学会委员,北京神经外科学分会副主任委员。师从中国著名神经介入专家凌锋教授和世界介入神经放射学联合会主席Luc PICARD教授。专长于脑、脊髓血管病的介入治疗。在国内或国际上首先开展或报道的工作有:脑动静脉畸形动物模型、血流动力学模型的建立和栓塞研究,电解可脱式弹簧圈栓塞治疗颅内动脉瘤,颅内动脉瘤栓塞标准的专题研究,三维脑血管造影成像在颅内动脉瘤诊断和治疗的应用,支架置入术治疗颅内动脉狭窄,脑保护装置下颈动脉和椎动脉狭窄的血管内扩张和支架置入治疗等。

David S. Liebeskind, M.D.
Professor of Neurology at the University of California, Los Angeles (UCLA), Director of the UCLA Stroke Center, Director of the Neurovascular Imaging Research Core, leading global efforts to advance data science and precision medicine of stroke imaging for prevention, acute therapies and recovery after stroke.
Director of the UCLA Cerebral Blood Flow Laboratory, Director of Outpatient Stroke and Neurovascular Programs and Director of the UCLA Vascular Neurology Residency Program, training the next generation of vascular neurologists and stroke experts.
通讯作者

焦力群,主任医师,教授。
首都医科大学宣武医院介入放射科主任,神经外科副主任,脑血运重建中心主任,博士生导师。
中国医师协会神经介入专业委员会副主委;国家卫健委继教中心神经介入专委会主委;国家卫健委脑防委缺血性卒中外科专委会主委;国家卫健委脑防委缺血性卒中介入专委会副主委;《中国脑血管病杂志》主编;中央保健会诊专家;北京介入医学会副会长等职务。
毕业于山东医科大学,先后师从于朱树干教授和凌锋教授,获得神经外科硕士和博士学位,并在鲍圣德教授的指导下,在北京大学完成博士后研究。
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#SSI#
50
#颅内动脉狭窄#
53
#宣武医院#
59
#动脉狭窄#
62
#Cas#
58
厉害👍
49
JAMA上文章都是顶级的,谢谢梅斯及时上新
49