Circ-Heart Fail:中国城市心衰患病率和发病率分析
2021-08-31 MedSci原创 MedSci原创
HF给我国卫生系统带来了相当大的负担,急需开发针对HF防治的策略。
在中国,关于心力衰竭(HF)发病率和患病率的大型和基于人群的研究很少。

近日,心血管领域权威杂志Circ-Heart Fail上发表了一篇研究文章,该研究旨在估计中国HF的患病率、发病率和医疗成本。

研究人员使用2017年来自中国6个省份的5000万名25岁以上参加全国城镇职工基本医疗保险的个体进行了一项基于人群的研究。2017年被诊断为HF(国际疾病分类代码和诊断文本)的个体为事件病例。研究人员通过对2010年中国人口普查人群进行年龄标准化来计算标准化率。
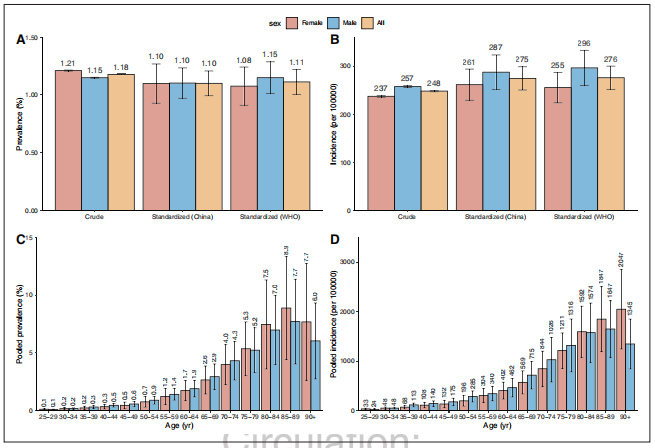 HF的年龄标准化患病率和发病率分别为1.10%(男性和女性为1.10%),每100000人每年有275人(男性287人,男性261人),分别有1210万名HF患者和300万名新发HF患者。患病率和发病率都随着年龄的增长而增加(25-64、65-79和80岁人群的患病率分别为0.57%、3.86%和7.55%)。HF患者的人均住院费用为4406.8美元,住院人数≥3次的比例为40.5%。HF患者的人均门诊费用为892.3美元。
HF的年龄标准化患病率和发病率分别为1.10%(男性和女性为1.10%),每100000人每年有275人(男性287人,男性261人),分别有1210万名HF患者和300万名新发HF患者。患病率和发病率都随着年龄的增长而增加(25-64、65-79和80岁人群的患病率分别为0.57%、3.86%和7.55%)。HF患者的人均住院费用为4406.8美元,住院人数≥3次的比例为40.5%。HF患者的人均门诊费用为892.3美元。
由此可见,HF给我国卫生系统带来了相当大的负担,急需开发针对HF防治的策略。
原始出处:
Hua Wang,et al.Prevalence and Incidence of Heart Failure Among Urban Patients in China: A National Population-Based Analysis.Circulation:heart failure.2021.https://www.ahajournals.org/doi/10.1161/CIRCHEARTFAILURE.121.008406
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言










#发病率#
29
#患病率#
21
#ART#
20
#HEART#
0
学习了
64