Eur Urol:前列腺特异性膜抗原和氟尿嘧啶转运体基因与原发性前列腺癌的不同临床特征和分子亚型有关
2021-04-29 AlexYang MedSci原创
在美国,基于8F-氟尿嘧啶的正电子发射断层扫描(PET)成像推荐用于前列腺癌治疗后的生化复发(BCR)。然而,基于前列腺特异性膜抗原(PSMA)的PET成像在世界范围内更为普遍,且由国际指南的支持,目
在美国,基于8F-氟尿嘧啶的正电子发射断层扫描(PET)成像推荐用于前列腺癌治疗后的生化复发(BCR)。然而,基于前列腺特异性膜抗原(PSMA)的PET成像在世界范围内更为普遍,且由国际指南的支持,目前在美国已被食品和药物管理局批准用于原发性前列腺癌的初始分期。

关于PSMA靶向PET/计算机断层扫描(CT)与18F-氟尿嘧啶PET/CT检测到的病变的分子特征知之甚少。最近,有研究人员调查了18000多份根治性前列腺切除术标本队列中PSMA(FOLH1)和氟尿嘧啶转运基因LAT1-4和ASCT1/2的表达情况,以及它们与临床结果的关系。
结果发现,在前列腺癌中,PSMA和除一种fluciclovine转运体基因外的所有基因的表达都高于良性组织的表达。PSMA的表达与格里森评分(GS)≥8和淋巴结受累(LNI)有关,并与Decipher风险评分呈线性正相关。相比之下,氟尿嘧啶转运体LAT2、LAT3和ASCT2的表达与GS≥8、LNI和Decipher高分负相关。PSMA表达的最高分位数与最差的无转移生存期(MFS)有关,而LAT3和ASCT2表达的最低分位数与最差的MFS有关。
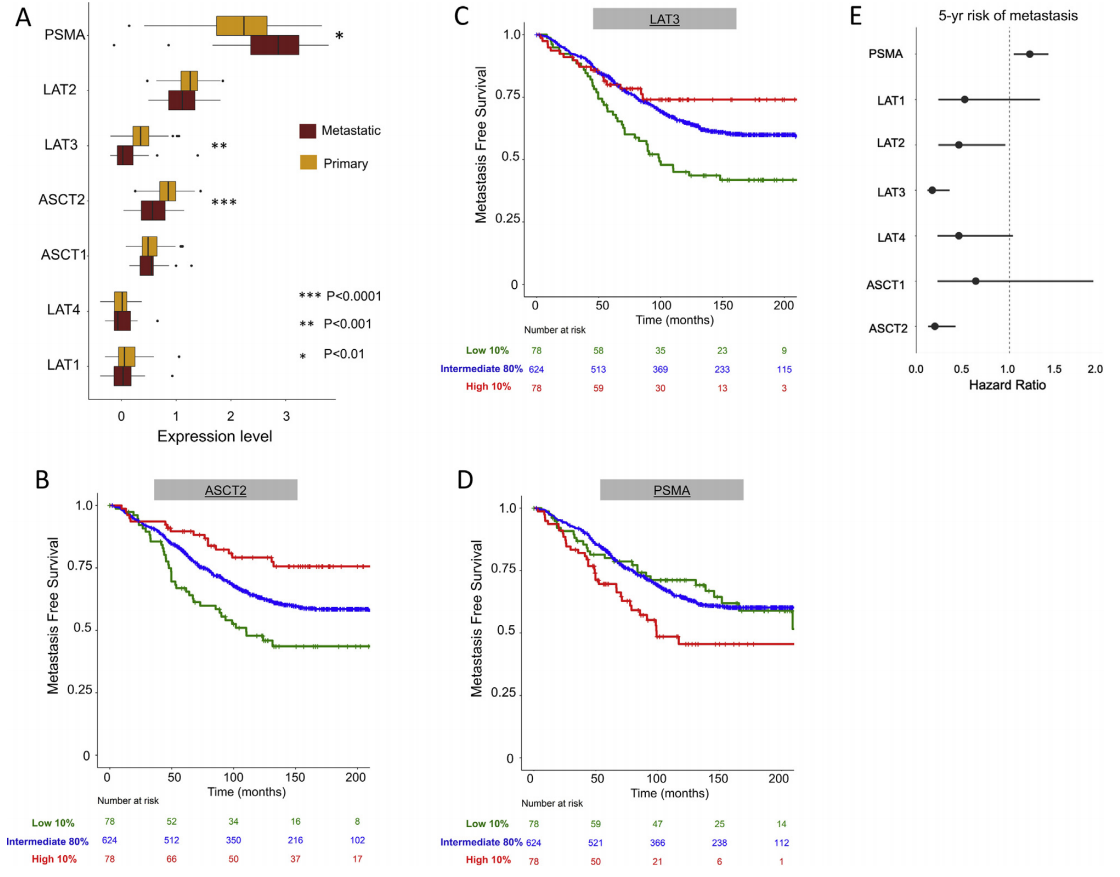
放射性示踪靶表达及与转移的关系
最后。研究人员指出,PSMA基因的表达(基于PSMA的示踪剂)与较差的临床结果有关,而ASCT2、LAT2和LAT3基因的表达(氟尿嘧啶示踪剂)则与较好的结果有关。
原始出处:
Carissa E Chu, Mohammed Alshalalfa, Martin Sjöström et al. Prostate-specific Membrane Antigen and Fluciclovine Transporter Genes are Associated with Variable Clinical Features and Molecular Subtypes of Primary Prostate Cancer. Eur Urol. Apr 2021
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#临床特征#
39
#前列腺特异性膜抗原#
37
#转运#
22
#特异性#
31
#原发性#
24
还不错
56
#分子亚型#
35
#氟尿嘧啶#
34
#抗原#
29
有意思的研究~
46