JACC:新晋“坏”血脂LPa升高居然会增加心房颤动的风险
2022-04-22 MedSci原创 MedSci原创
Lp(a)是房颤发展过程中的一个潜在的因果媒介,这表明Lp(a)的影响延伸至整个心肌组织。
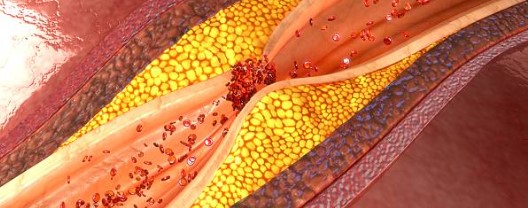
1963年,遗传学家Kare Berg发现了一种与低密度脂蛋白胆固醇(LDL-C)相似的脂蛋白颗粒,将其命名为脂蛋白(a)(LPa)。在过去的十年里,一些大型的当代研究重燃了这种兴趣,他们发现无论是从观察上还是从人类遗传学的因果关系上,高LPa水平与心肌梗死和主动脉瓣狭窄的风险增加有关。
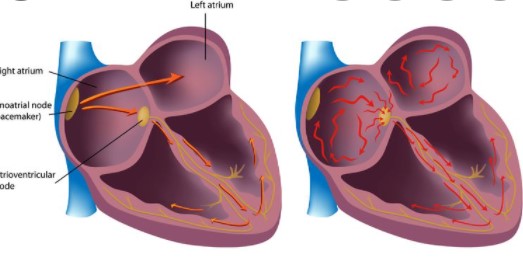
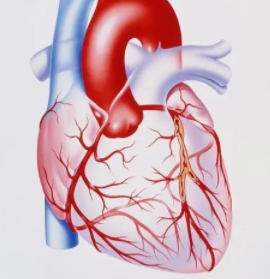
心房颤动(AF)是一种心律失常,与中风、心力衰竭和死亡的风险升高有关。然而,需要明确对其心血管并发症有辅助治疗作用的预防性疗法。Lpa是公认的动脉粥样硬化性心血管疾病(ASCVD)的危险因素,其本身会增加房颤风险,但Lpa是否是独立于ASCVD的房颤的因果介导因素仍是未知数。
为了调查Lp(a)在房颤中的作用以及它是否独立于ASCVD,来自加拿大David Braley心脏、血管和中风研究所的专家开展了相关研究,结果发表在JACC杂志上。
研究人员在英国生物库(N = 435579)中测试了测量和遗传预测的Lp(a)水平与20,432例发生的房颤的关系。通过使用来自公开的全基因组关联研究(N = 1145375)的房颤汇总级数据进行孟德尔随机化分析。
在英国生物库中,Lp(a)每增加50 nmol/L(23 mg/dL)与发生房颤的风险增加有关。其中使用测量的Lp(a)(HR=1.03;95%CI:1.02-1.04;P=1.65×10-8)与使用遗传预测的Lp(a)(OR=1.03;95%CI:1.02-1.05;P=1.33×10-5)风险均增加3%。
使用独立数据进行的孟德尔随机化分析复制了这一效应(每增加50 nmol/L,HR=1.04;95% CI:1.03-1.05)。但没有证据表明低密度脂蛋白胆固醇或甘油三酯有风险推断作用,只有39%(95% CI:27%-73%)的Lp(a)风险是通过ASCVD介导的,这表明Lp(a)部分影响房颤,而不是其对ASCVD的已知影响。

该研究结果表明,Lp(a)是房颤发展过程中的一个潜在的因果媒介,这表明Lp(a)的影响延伸至整个心肌组织。
参考文献:
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言














#JACC#
76
#ACC#
31
#LPA#
48
#心房#
37