JACC:双重抗血小板药物治疗对冠脉支架植入术后缺血风险的影响
2019-02-20 不详 MedSci原创
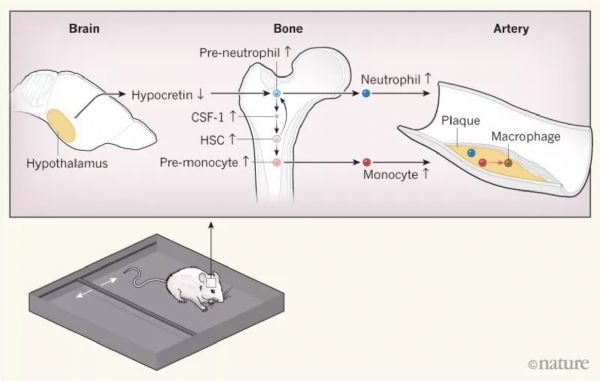
复杂型经皮冠脉介入治疗(PCI)与更高的缺血性风险相关,可通过长期的双重抗血小板药物治疗(DAPT)缓解,但这又会增加患者出血的风险。本研究的目的旨在评估冠脉支架植入后DAPT治疗期间的缺血和出血风险。本研究中的复杂型PCI定义为≥3个支架的植入或为≥3个靶病变的治疗,分叉口的支架植入和/或支架长度>6cm,和/或慢性完全闭塞血运重建。最终共纳入了来自8个临床随机试验的14963名患者,其中311
本文系梅斯医学(MedSci)原创编译整理,转载需授权!
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言









#血小板药物#
46
#抗血小板药#
43
#冠脉支架#
48
#JACC#
29
#支架植入#
50
#ACC#
34
#植入#
31
#支架植入术#
33
有高出血风险的复杂PCI是不是就不用双抗了,这违背原则吗?
69