JCC: 炎症性肠病女性剖腹产后的产后手术并发症发生率增加
2021-11-03 MedSci原创 MedSci原创
溃疡性结肠炎和克罗恩病通常会影响女性的生育。但近年来,炎性肠病(IBD)研究领域的进展使许多女性患者成功妊娠,这使得生育这个家庭计划得到消化科医师和患者的共同关注。
炎症性肠病 (IBD) 通常会在患者育龄期间被诊断出来,通常与怀孕时间重合。IBD女性患者比一般人群的剖腹产率高,但其原因尚不清楚。女性剖腹产的风险包括感染、产后出血、麻醉反应、血栓、伤口感染、手术损伤等。这些风险在患有IBD的女性中可能会明显增加,尤其是那些使用免疫抑制剂或处于疾病活动期。本项研究的目标是确定接受剖腹产而不是阴道分娩的炎症性肠病 (IBD) 女性的产后 30 天手术并发症发生率之间的差异。

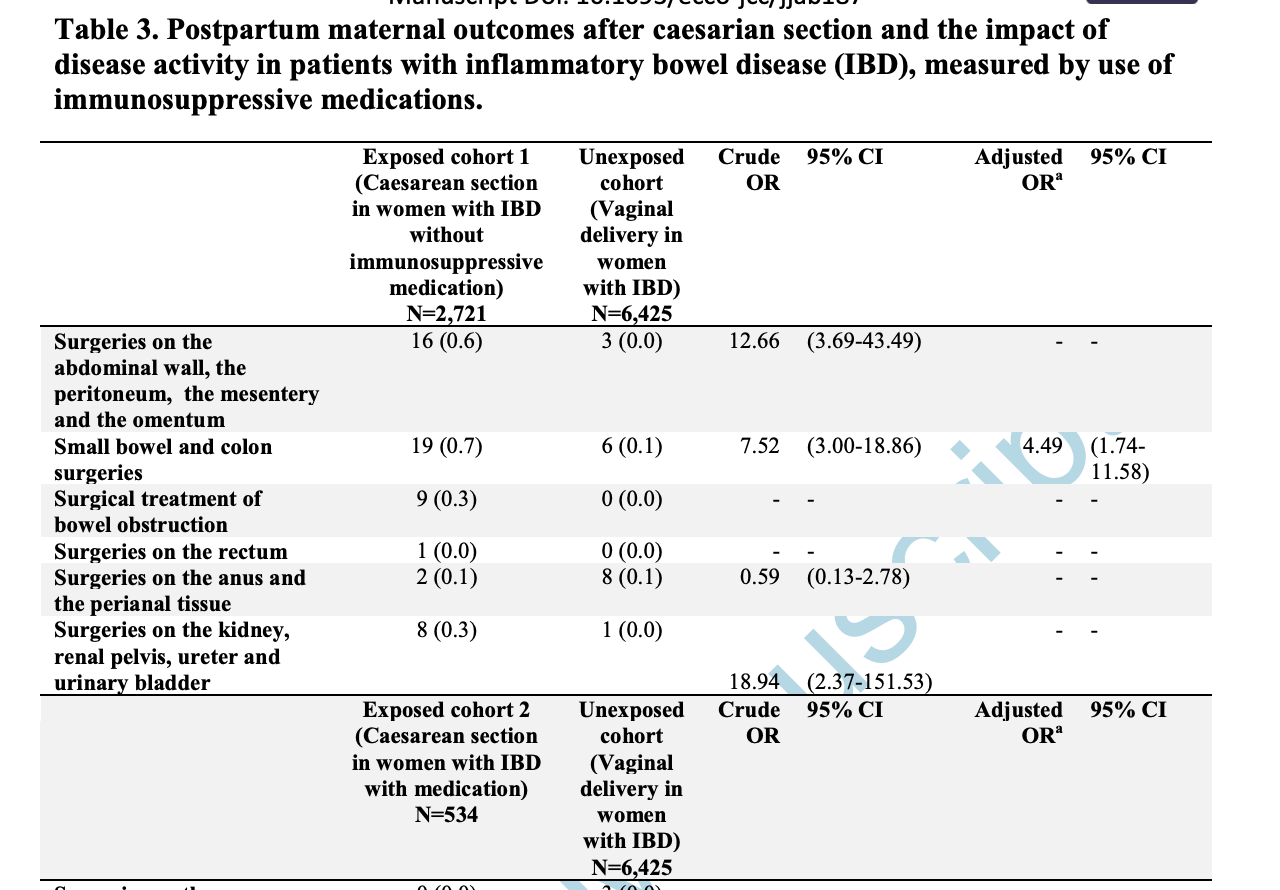
研究人员收集了1997年1月1日至2015年12月的生育的妇女资料,将所有剖腹产或阴道分娩的 IBD 母亲纳入本项研究中。然后比较了产后 30天产妇腹部和会阴部的手术结果,并针对多个混杂因素进行了调整。研究人员对急诊与选择性剖腹产以及免疫抑制疗法对产后并发症的影响。

研究结果显示在患有IBD的女性中,有2.1%的剖腹产妇女 (n=3,255) 和 0.3% 的阴道分娩妇女 (n=6,425) 有手术并发症。剖腹产的 IBD 女性更有可能进行小肠和结肠手术((aOR) 5.00,95% CI 2.00-12.51)。无论是急性 (aOR 4.51, 95% CI 1.48-13.76) 还是择期 (aOR 6.52, 95% CI 2.45-17.33) 剖腹产,都发现了类似的结果。研究人员还发现无论是否使用免疫抑制剂(使用免疫抑制剂的 aOR:8.79,95% CI 2.86-27.05)和(未使用免疫抑制剂的 aOR:4.49,95% CI 1.74-11.58),剖腹产术后的手术风险都会增加。
本项研究证实与阴道分娩相比,无论剖腹产是出于急诊还是选择性的原因或者在分娩前使用免疫抑制剂,IBD女性剖腹产术后发生手术并发症的风险增加。因此许多消化科医师认为,对于无复杂疾病的克罗恩病妊娠妇女,在决定其分娩方式时,更应该 慎重。
原始出处:
Sonia Friedman. et al. Postpartum surgical complications in women with inflammatory bowel disease after caesarian section: A Danish nationwide cohort study. Journal of Crohn's and Colitis.2021.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言










#剖腹产##炎症性肠病#
84
#发生率#
31
#并发#
45
#手术并发症#
49
#炎症性#
42