Blood:羟基脲 vs 聚乙二醇化IFN-α 治疗原发性血小板增多症/真性红细胞增多症
2022-05-19 MedSci原创 MedSci原创
羟基脲和聚乙二醇化 IFN-α 都可以有效治疗原发性血小板增多症和真性红细胞增多症
原发性血小板增多症 (ET) 和真性红细胞增多症 (PV) 是一类骨髓增生性肿瘤 (MPN),其特征是携带特定的驱动突变。这类疾病患者的治疗目标是通过使血细胞计数正常化来减少血栓事件。
对于高血管并发症风险的原发性血小板增多症和真性红细胞增多症患者,羟基脲 (HU) 和干扰素-α (IFN-α) 是最常用的细胞减灭剂。尽管经常使用,但 IFN-α 与羟基脲相比孰优孰劣尚未明确。
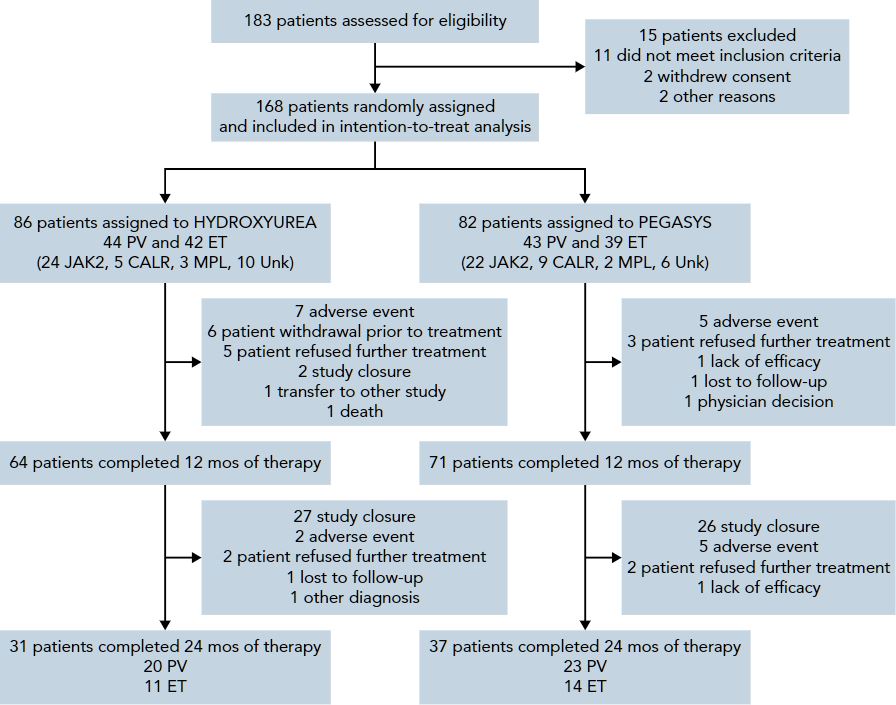
Myeloproliferative Disorders Research Consortium 112研究是一项由调查员发起的、随机化的3期临床试验,旨在对比 HU 与聚乙二醇化 IFN-α(PEG)在初治高危型 ET/PV 患者中的疗效和安全性。
研究流程
高风险定义(包含以下因素的任一项):有血栓栓塞史、年龄>60岁、有出血史(ET患者)、血小板计数>1500x109/L(ET)或>1000x109/L(PV)、血管舒缩症状(红斑性肢痛、严重的偏头痛)、明显或有症状的脾肿大及合并需要药物干预的糖尿病或高血压。受试患者被随机1:1分至两组,接受 HU(500mg*2次/天)或 PEG(45ug/周,每月增加45ug,最大剂量 180ug)干预。主要终点是12个月时的完全缓解率(CR)。
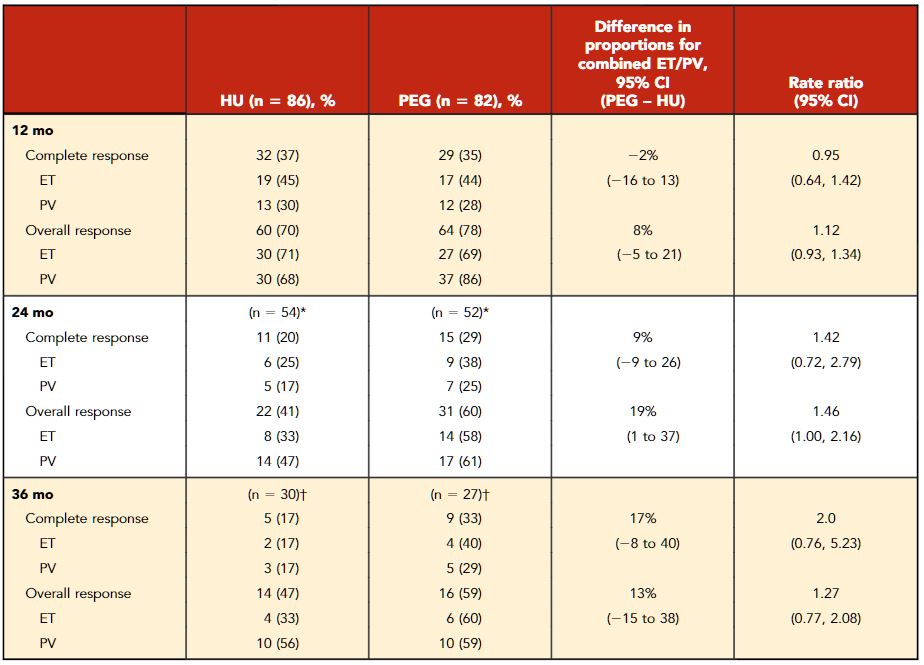
治疗反应
共招募了168位患者,中位治疗了81.0周。12个月时羟基脲组和聚乙二醇化 IFN-α 组的完全缓解率分别是37%和35%(p=0.80)。第24个月至第36个月期间,羟基脲组的完全缓解率从20%降到了17%,聚乙二醇化 IFN-α 组的完全缓解率从29%升高到了33%。
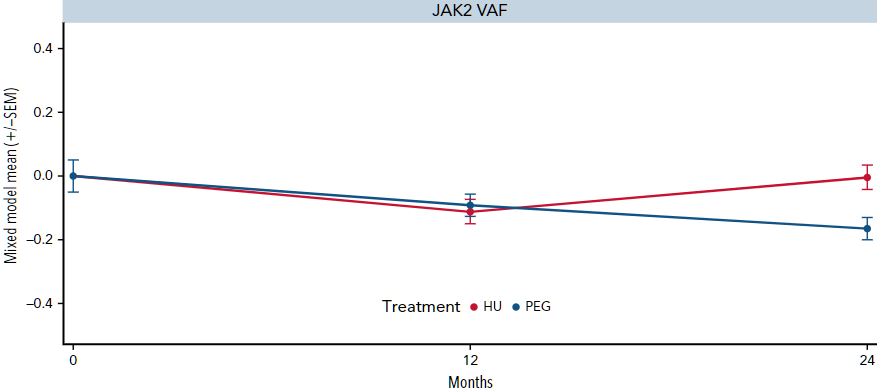
JAK2变异负荷的变化
第24个月时,PEG组的JAK2V617F减少更显著,但羟基脲组的组织病理学缓解率更高。两组的血栓事件和疾病进展均不常见,但聚乙二醇化 IFN-α 组的3/4级不良事件的发生率相对更高(46% vs 28%)。
总之,该研究结果提示,羟基脲和聚乙二醇化 IFN-α 都可以有效治疗原发性血小板增多症和真性红细胞增多症,在限制高风险患者的血栓事件和疾病进展方面没有差异。随着治疗时间的延长,聚乙二醇化 IFN-α 在使血细胞计数正常化和减少驱动突变负荷方面更有效,而羟基脲在组织病理学反应方面更具优越性。
原始出处:
John Mascarenhas, et al. A randomized phase 3 trial of interferon-α vs hydroxyurea in polycythemia vera and essential thrombocythemia. Blood (2022) 139 (19): 2931–2941. https://doi.org/10.1182/blood.2021012743.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言













#血小板增多症#
27
#乙二醇#
51
#原发性#
40
#红细胞#
44
#羟基脲#
34
#IFN#
41
#红细胞增多症#
46
#原发性血小板增多症#
43
认真学习了
50