A&R:软骨寡聚基质蛋白(COMP)的抗体在小鼠中具有致病性,并且可能与类风湿性关节炎具有临床相关性
2022-06-12 MedSci原创 MedSci原创
该研究结果为将致病性抗COMP抗体与软骨结合提供了结构基础。识别的表位可以是瓜氨酸化的,RA患者中针对该表位的抗体水平升高并与较高的疾病活动度相关,这表明抗COMP抗体在部分RA患者中具有致病作用。
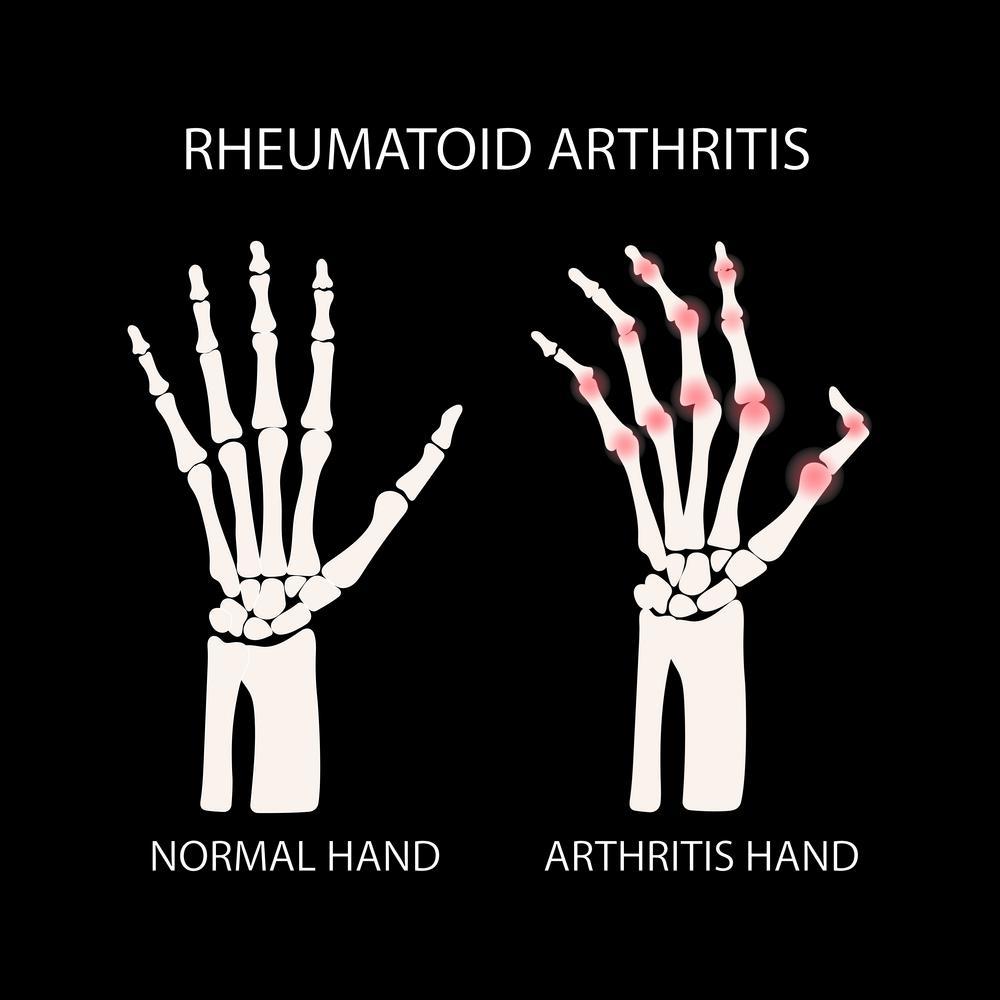
目的:软骨寡聚基质蛋白(COMP)是类风湿性关节炎(RA)和关节炎实验模型中的自身抗原。COMP的具体功能仍未确定,但似乎通过与胶原原纤维和其他基质成分(如蛋白聚糖和纤连蛋白)的相互作用在细胞外基质(ECM)的组装和稳定中发挥结构作用。本研究旨在调查抗COMP抗体的结构、功能和相关性。
方法:研究人员使用被动转移实验研究了单克隆抗COMP抗体在小鼠中的致病性,并使用免疫组织化学染色探索了抗COMP抗体与软骨的相互作用。单克隆抗体15A11与其特异性COMP表位P6复合物的相互作用通过X射线晶体学测定。酶联免疫吸附测定和表面等离子体共振技术用于研究钙离子与15A11结合的调节。在一个大型瑞典RA患者队列中评估了抗COMP P6 表位及其瓜氨酸变异的血清 IgG 的临床相关性和价值。
结果:鼠单克隆抗COMP抗体15A11在幼稚小鼠中诱导关节炎。15A11-P6复合物的晶体结构解释了抗体如何与COMP结合,而COMP可以被钙离子调节。此外,与健康对照相比,在RA患者中可检测到对COMP P6肽及其瓜氨酸化变异具有特异性的血清IgG,并且与更高的疾病活动评分相关。
结论:该研究结果为将致病性抗COMP抗体与软骨结合提供了结构基础。识别的表位可以是瓜氨酸化的,RA患者中针对该表位的抗体水平升高并与较高的疾病活动度相关,这表明抗COMP抗体在部分RA患者中具有致病作用。
出处:Ge, C., Tong, D., Lönnblom, E., Liang, B., Cai, W., Fahlquist-Hagert, C., Li, T., Kastbom, A., Gjertsson, I., Dobritzsch, D. and Holmdahl, R. (2022), Antibodies to Cartilage Oligomeric Matrix Protein Are Pathogenic in Mice and May Be Clinically Relevant in Rheumatoid Arthritis. Arthritis Rheumatol, 74: 961-971. https://doi.org/10.1002/art.42072
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言









#致病性#
40
#相关性#
24
#基质#
30
#关节炎#
24
#类风湿#
0
#风湿性关节炎#
51
认真学习~~
35
学习学习学习学习学习学习学习学习学习学习学习学习学习学习学习学习学习学习学习学习学习学习
43