孤独症谱系障碍(孤独症)是一种慢性神经发育疾病,具有高度可变的临床表现。除了自闭症的核心表型表现(社交沟通困难和兴趣受限/重复行为)之外,新出现的证据提示,近一半的自闭症患者有胃肠道症状。此外,与对照儿童相比,自闭症儿童被诊断为克罗恩病的可能性约高47%,被诊断为溃疡性结肠炎(UC)的可能性约高94%。
克罗恩病和UC是炎症性肠病(IBD)的主要亚型,IBD是一种与免疫系统失调、肠道微生物组改变、微量营养素吸收不良和贫血相关的慢性疾病。有证据表明,IBD的这些特征可能是与自闭症相关的围产期因素。在此基础上,可以假设父母IBD与儿童自闭症之间的潜在联系。迄今为止的证据尚不明确,该领域4项基于登记系统的研究中只有1项表明母亲UC与儿童自闭症之间存在关联。此外,任何关联的基础病因尚不清楚。
英国布里斯托大学的Christina Dardani研究团队在nature medicine期刊发表重要研究成果。通过四项互补的遗传和流行病学研究发现,父母,特别是母亲,罹患IBD与孩子罹患ASD风险增加密切相关。

该研究进行了4项补充研究,以调查父母IBD与儿童自闭症之间的关联,并阐明了其潜在病因。
(1)在瑞典的一个全国性队列中,父母诊断的IBD与儿童自闭症之间的关联;
(2)利用全基因组关联研究(GWAS)汇总统计分析IBD与孤独症的遗传相关性;
(3)在一个大型英国出生队列中,母亲对IBD的遗传易感性与儿童的自闭症特征之间的多基因关联;
(4)使用双向双样本孟德尔随机化(MR)研究IBD的遗传易感性对自闭症的潜在因果关系和反向因果关系的可能性。
表2. 母亲或父亲诊断为任何IBD、UC、克罗恩病或其他IBD与儿童自闭症诊断之间的关联

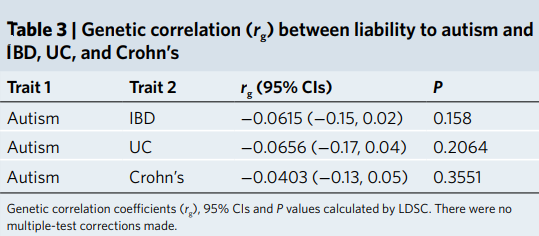
表3.自闭症易感性与IBD、UC和克罗恩病之间的遗传相关性(rg)
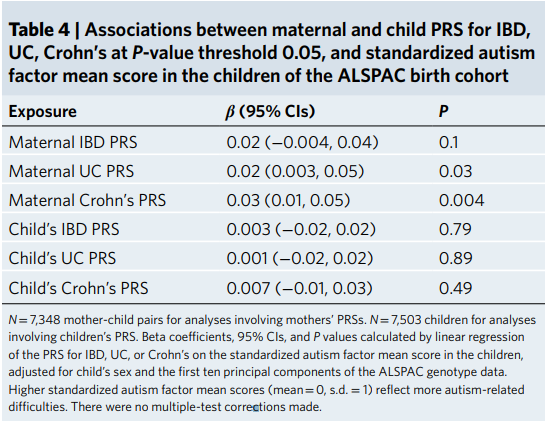
父母和儿童纵向研究的多基因风险评分分析表明,母亲对IBD的遗传易感性与儿童的自闭症特征之间存在关联。
表4. 在ALSPAC出生队列中,母亲和儿童PRS与IBD、UC、克罗恩病(p阈值为0.05)和标准化孤独症因子平均评分之间的关联
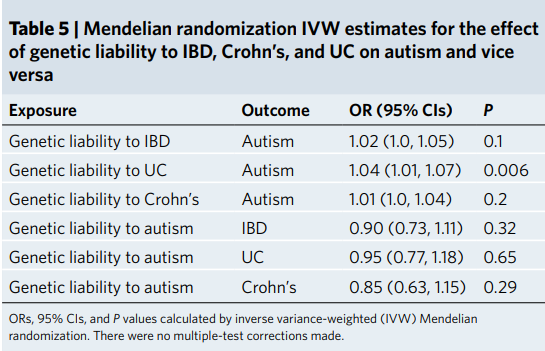
两样本孟德尔随机化分析证明了IBD(尤其是溃疡性结肠炎)的遗传易感性对自闭症的潜在因果效应。
表5.孟德尔随机化IVW评估了IBD、克罗恩病和UC的遗传易感性对自闭症的影响,反之亦然
连锁不平衡评分回归未显示IBD和孤独症之间存在遗传相关性。
通过对这四种互补方法的证据进行三角分析,发现了父母(尤其是母亲)IBD与儿童自闭症之间潜在因果关系的证据。可能与围生期免疫失调、微量营养素吸收不良和贫血有关。
原文出处
Parental inflammatory bowel disease and autism in children. Nat Med. 2022 Jul;28(7):1406-1411. doi: 10.1038/s41591-022-01845-9. Epub 2022 Jun 2. PMID: 35654906; PMCID: PMC9307481.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











#Nat#
52
我已经学习了
21
#自闭#
40
#Med#
34