JCEM:新型糖尿病亚组身体健康与心血管危险因素的关系
2021-11-14 MedSci原创 MedSci原创
尽管所有亚组的内皮功能相当,但SIRD亚组的体能最低。值得注意的是,与其他糖尿病亚组相比,SAID在糖尿病诊断后的第一年内心血管风险最低。
缺乏运动会促进胰岛素抵抗,并增加患糖尿病和心血管疾病的风险。最近引入的基于简单临床测量的聚类可确定了具有不同糖尿病相关合并症和并发症风险的糖尿病亚组(聚类)。

近日,内分泌和代谢性疾病领域权威杂志Journal of Clinical Endocrinology & Metabolism上发表了一篇研究文章,该研究旨在明确糖尿病亚组和葡萄糖耐受对照组(CON)之间的体能和心血管风险差异。研究人员假设严重的胰岛素抵抗性糖尿病(SIRD)亚组与较低的身体素质和增加的心血管风险有关。

研究人员对746名近期发病的糖尿病患者(糖尿病病程<12个月,年龄为18-69岁)和德国糖尿病研究(GDS)的74名CON参与者的身体健康和心血管风险进行了分析,该研究是一项前瞻性纵向队列研究。该研究的主要结局指标包括身体健康(来自肺活量计的最大摄氧量)、内皮功能(血流和硝酸甘油介导的扩张)和心血管风险评分(冠心病弗雷明汉风险评分(FRS-CHD)和动脉粥样硬化心血管疾病(ASCVD)风险评分)。
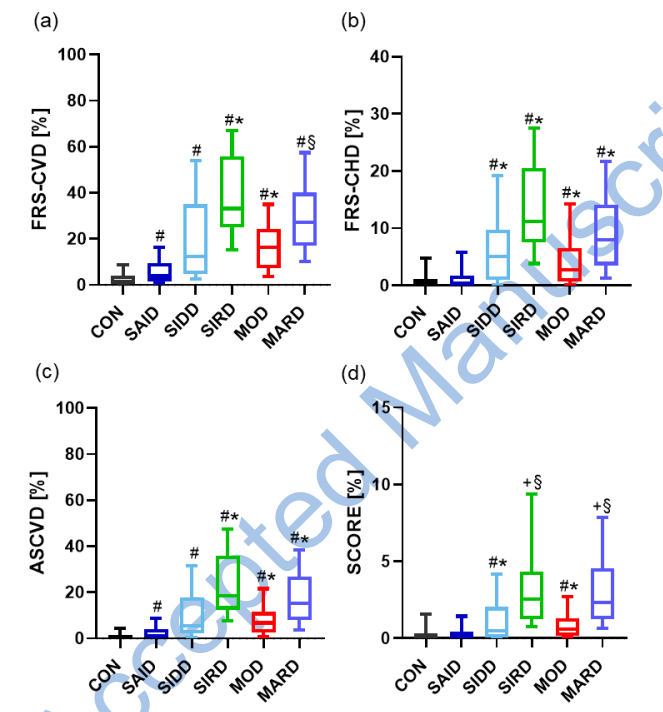
SIRD患者的VO2max较低,相比于CON、严重自身免疫性糖尿病(SAID)(均p<0.001)和轻度年龄相关糖尿病(MARD)(p<0.01)亚组,但在调整年龄、性别和BMI后,其与严重胰岛素缺乏型糖尿病(SIDD)(p=0.98)和中度肥胖相关糖尿病(MOD)亚组(p=0.07)相比没有差异。所有组的内皮功能相似,而SAID亚组的FRS-CHD和ASCVD低于SIRD、MOD和MARD亚组(所有p<0.001)。
由此可见,尽管所有亚组的内皮功能相当,但SIRD亚组的体能最低。值得注意的是,与其他糖尿病亚组相比,SAID在糖尿病诊断后的第一年内心血管风险最低。
原始出处:
Nina Saatmann.et al.Physical fitness and cardiovascular risk factors in the novel diabetes subgroups.JCEM.2021.https://academic.oup.com/jcem/advance-article/doi/10.1210/clinem/dgab810/6423502
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#JCEM#
43
#血管危险因素#
46
#JCE#
37
#心血管危险因素#
36
#身体健康#
57
#心血管危险#
37
已读已读已读已读已读已读已读已读已读已读已读已读已读已读
38