Comput Math Methods Med:牙周治疗可有效降低慢性牙周炎患者促炎性细胞因子的水平
2022-08-16 MedSci原创 MedSci原创
牙周炎作为一种常见的侵犯牙龈和牙周组织的慢性炎症,也是一种以进行性附着丧失和牙槽骨丧失为特征的慢性感染性疾病。在慢性牙周炎(CP)的发展过程中,患者血清和龈沟液(GCF)中炎症因子的水平会发生变化。
牙周炎作为一种常见的侵犯牙龈和牙周组织的慢性炎症,也是一种以进行性附着丧失和牙槽骨丧失为特征的慢性感染性疾病。在慢性牙周炎(CP)的发展过程中,患者血清和龈沟液(GCF)中炎症因子的水平会发生变化。近日,发表于Comput Math Methods Med的一项荟萃分析系统地评估了牙周治疗对CP患者GCF和血清中促炎症细胞因子(IL-6、TNF-α和IL-8)水平的影响。
研究人员系统检索了PubMed、Web of Science、Embase、中国国家知识基础设施(CNKI)和万方数据库中收录的2015年至2020年间比较牙周治疗(实验组)和对照组的细胞因子水平的随机对照试验。此外,还对相关文章、会议论文和摘要的参考文献列表进行了额外的检索,以挖掘出其他潜在的文章。
结果,共纳入13项研究,包括1220名患者,其中实验组有630例,对照组有590例。荟萃分析结果显示,与治疗前相比,实验组的GCF(SMD=-2.88,95%CI(-3.68,-2.09),P<0.001)和血清(SMD=-1.27,95%CI(-1.72,-0.81),P<0.001)中的IL-6水平明显降低。此外,实验组的GCF(SMD = -2.08,95% CI(-3.40,-0.76),P < 0.001)和血清(SMD = -1.73,95% CI(-2.76,-0.70),P < 0。 001)中的IL-8水平在牙周治疗后减少,但更多的是观察到治疗后GCF(SMD = -3.98,95% CI(-5.23,-2.73),P < 0.001)和血清(SMD = -1.80,95% CI(-3.16,-0.45),P < 0.001)的TNF-α水平的下降。
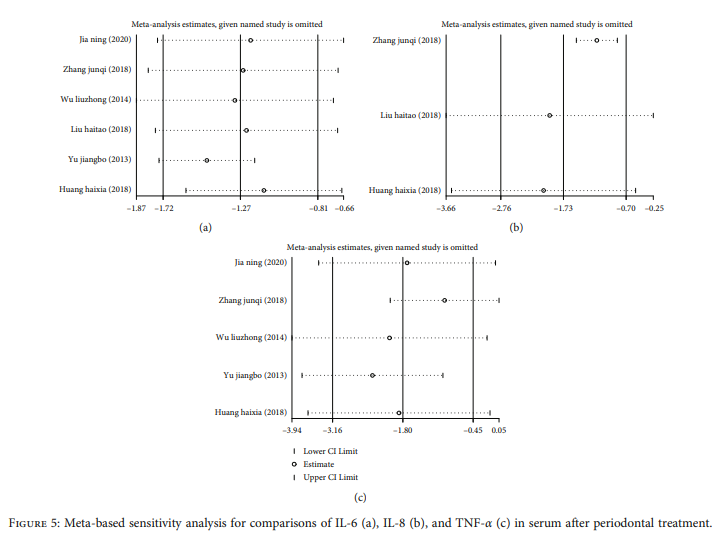
综上所述,该研究结果表明,牙周治疗后,CP患者GCF和血清中的促炎症细胞因子与治疗前相比明显下降,疗效显著,因此值得临床推广牙周治疗。
原始出处:
Jiahui Ren, Hong Li. Effects of Periodontal Treatment on Levels of Proinflammatory Cytokines in Patients with Chronic Periodontitis: A Meta-Analysis. Comput Math Methods Med. 2022 Jul 26;2022:9349598. doi: 10.1155/2022/9349598.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#胞因子#
45
#MET#
41
#促炎#
50
#细胞因子#
39
#慢性牙周炎#
41
#牙周#
46
#牙周治疗#
55
#Med#
30