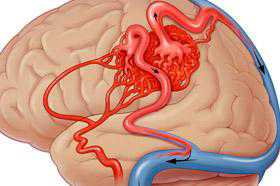
JAMA:未破裂的脑动静脉畸形保守治疗或介入治疗后的转归
2014-04-25 刘素梅 译 中国医学论坛报
对于未破裂的脑动静脉畸形(bAVMs),由于缺乏长期的比较数据,保守治疗是否优于介入治疗尚不清楚。来自英国爱丁堡市爱丁堡大学临床脑科学中心临床神经分部的鲁斯塔姆·阿勒沙希·萨洛曼等博士考察比较了bAVMs保守治疗与介入治疗的长期转归。 设计、场所和参与者 对204名年龄≥16岁的居民进行了基于人群的起始队列研究,他们均于1999-2003年或2006-2010年期间首次被确诊为未破裂的bAVMs
对于未破裂的脑动静脉畸形(bAVMs),由于缺乏长期的比较数据,保守治疗是否优于介入治疗尚不清楚。来自英国爱丁堡市爱丁堡大学临床脑科学中心临床神经分部的鲁斯塔姆·阿勒沙希·萨洛曼等博士考察比较了bAVMs保守治疗与介入治疗的长期转归。
设计、场所和参与者 对204名年龄≥16岁的居民进行了基于人群的起始队列研究,他们均于1999-2003年或2006-2010年期间首次被确诊为未破裂的bAVMs,且之后接受了12年的前瞻性随访。
治疗 保守治疗(无介入)对比介入治疗[任何血管内栓塞(疗法)、神经外科切除术或立体定位放射外科手术,单用或联合应用]。
主要转归与检测指标 为比较主要转归[任何原因引起的死亡或持续病残率,牛津残障量表(OHS)评分≥2、持续≥2年(0=无症状,6=死亡]和次要转归(非致死性症状性卒中或bAVM、相关动脉瘤或介入治疗引起的死亡)的发生率,(研究人员)进行了考克斯(Cox)回归分析,如果风险成比例,则对预后因素和基线不平衡进行多变量校正。
结果 在204例患者中,103例接受了介入治疗。与接受保守治疗者相比,接受介入治疗者较年轻,更可能有癫痫表现,有大bAVMs的可能性较小。中位随访6.9年(随访完成率为94%),随访的前4年内,保守治疗组患者进展至主要转归的发生率较低(36对39次事件,9.5对9.8次/100人-年,校正风险比为0.59,95%可信区间为0.35~0.99),但随后两组的发生率相似。在12年的随访期内,保守治疗组患者的次要转归发生率较低(14对38次事件,1.6对3.3次/100人-年,校正风险比为0.37,95%可信区间为0.19~0.72)。
结论 与相关性在年龄≥16岁、确诊有未破裂的bAVMs患者中,与接受介入治疗相比,接受保守治疗与治疗后12年内的临床转归较好相关。需要进行更长时间的随访研究,以了解这种相关性是否能够持续。
原始出处:
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言








#静脉#
25
#动静脉畸形#
0
#畸形#
35
#保守治疗#
32