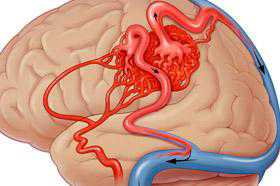
J Neurosurg:如何处理高级别脑动静脉畸形?
2016-06-04 MedSci MedSci原创
目前,脑动静脉畸形(AVM)的治疗主要是血管内栓塞、显微手术切除、立体定向放疗(SRS)和随访观察等几种手段的综合治疗。对于高级别的,即Spetzler-Martin分级在III至V级的AVM,其体积大、部位深或累及功能区,单纯手术切除风险很大。单次SRS的总放射剂量低,不适合用于高级别AVM。体积分割SRS(VS-SRS)将AVM畸形团分割为2-3个部分进行放疗,可以达到更高的放射剂量,但治愈率
目前,脑动静脉畸形(AVM)的治疗主要是血管内栓塞、显微手术切除、立体定向放疗(SRS)和随访观察等几种手段的综合治疗。对于高级别的,即Spetzler-Martin分级在III至V级的AVM,其体积大、部位深或累及功能区,单纯手术切除风险很大。单次SRS的总放射剂量低,不适合用于高级别AVM。体积分割SRS(VS-SRS)将AVM畸形团分割为2-3个部分进行放疗,可以达到更高的放射剂量,但治愈率仍不理想。美国加州大学旧金山分校神经外科的Adib A. Abla团队提出VS-SRS结合手术切除的治疗方案,结果发表在2015年2月的《J Neurosurg》上。
作者搜集自1992年至2012年间接受VS-SRS治疗的74例患者临床资料,包括Spetzler-Martin分级、补充Spetzler-Martin分级和改良Rankin评分(mRS)。AVM患者在治疗前均在由神经内外科医生、神经介入医生、放射肿瘤科医生和gamma刀技术员组成的多学科会议上进行讨论,对于不适合手术切除的高级别AVM,首先采用VS-SRS治疗。每次放疗靶标的体积小于8-10cm3,剂量大于17Gy,前后次放疗间隔3-6个月;放疗结束后12个月行MRI扫描,36个月行DSA检查。如果患者的Spetzler-Martin分级显著下降,则安排进一步手术切除术(图1)。
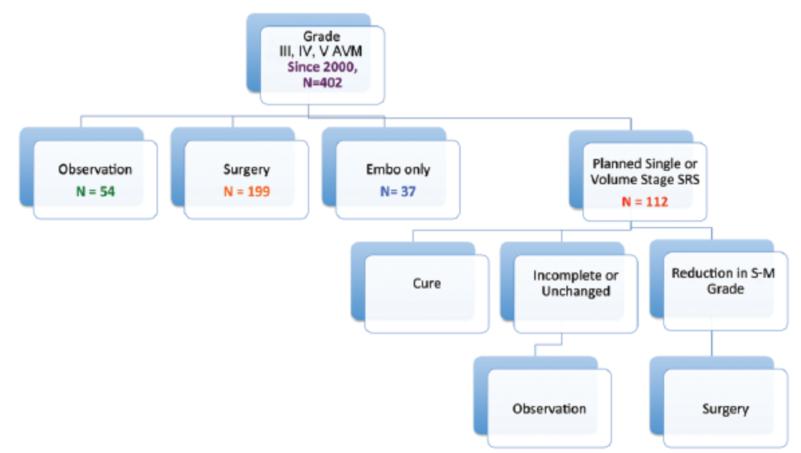
图1. III至V级AVM患者治疗流程图。Embo=栓塞;S-M=Spetzler-Martin评分。
在74例患者中, 8例(10.8%)获得治愈,50例(67.6%)未见明显疗效,16例(21.6%)进一步接受显微手术治疗。该16例患者平均年龄25岁;其中10例女性,6例男性;4例患者以AVM破裂出血为首发症状。在2~5次,平均2.7次的VS-SRS治疗之后,患者Spetzler-Martin分级、补充Spetzler-Martin分级和AVM平均直径分别由术前的4.0级、7.1级和5.0cm下降至2.5级、5.6级和3.0cm。其中,14例Spetzler-Martin分级等于或低于III级,13例补充Spetzler-Martin分级等于或低于6级,达到适合手术切除的指征(图2)。
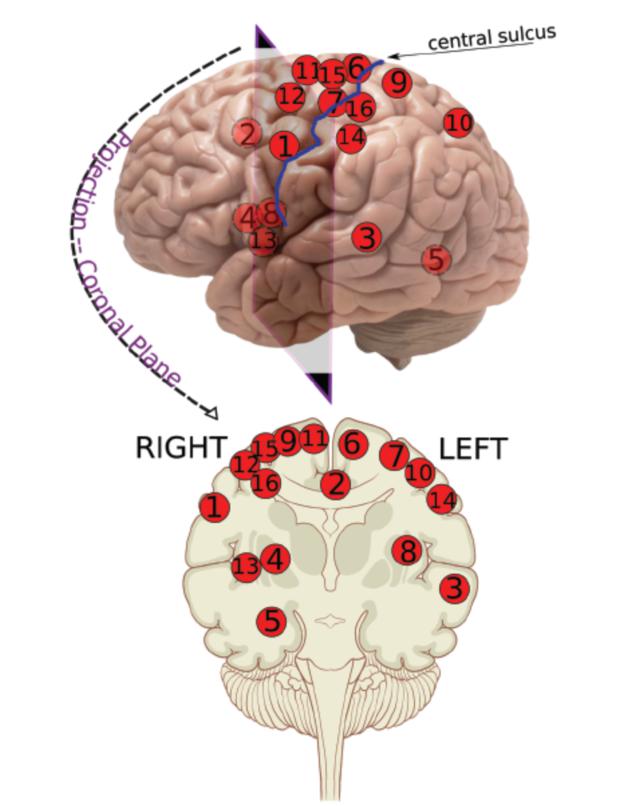
图2. 16名患者AVM的具体分布位置。
从VS-SRS治疗至显微手术切除的间隔时间为0.5-18.7年,平均5.7年。在此期间,4例患者AVM出血而接受手术,6例在手术切除前接受介入栓塞治疗。最终,1例因AVM位于感觉性语言中枢未全切除,其余15例(93.8%)均获得AVM全切除(图3)。
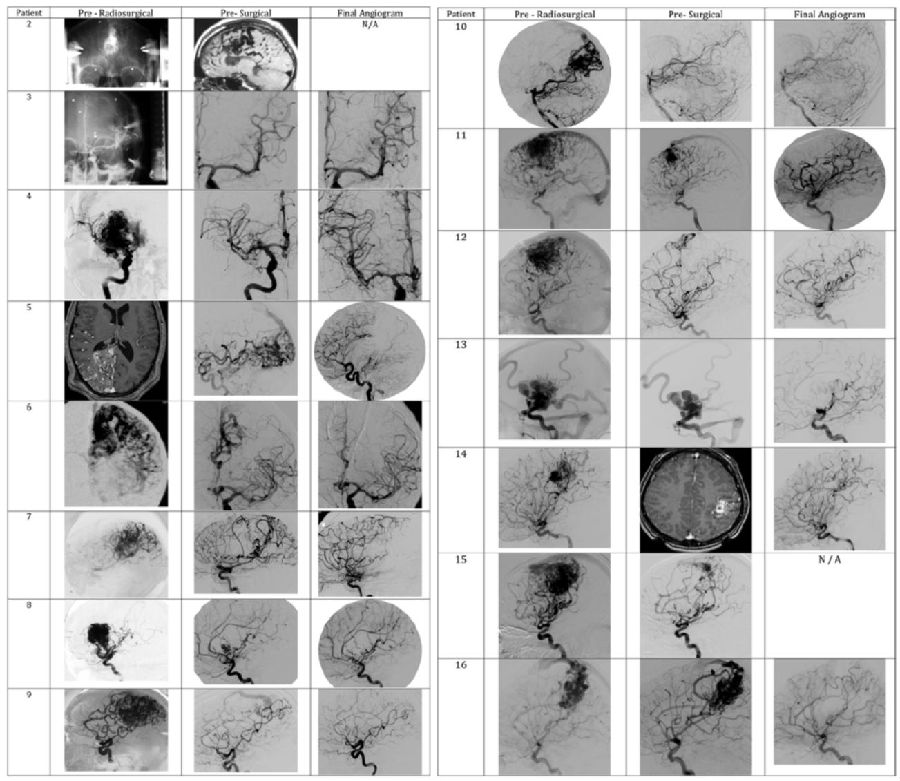
图3. 16例AVM患者VS-SRS前、手术切除前和术后最后一次随访时的影像学评估结果。
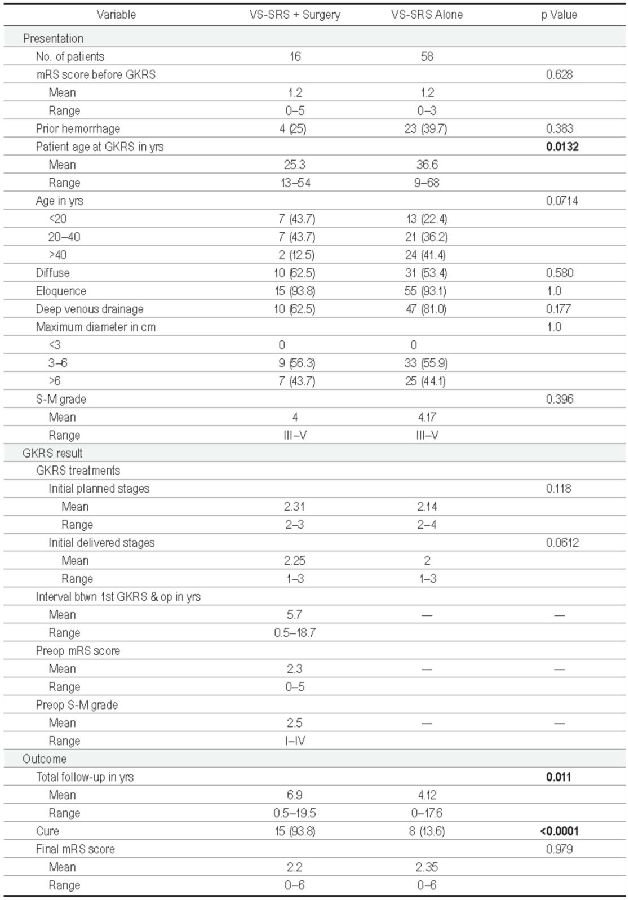
患者在VS-SRS前、手术切除前和最后一次随访时的平均mRS评分分别为1.2、2.3和2.2分。随访时间0.5-19.5年,平均为6.9年。其中,10例患者(62.5%)mRS评分0-1分,属良好;4例mRS 3分,属不佳,其中1例在VS-SRS治疗后病情加重,1例在VS-SRS起效期间AVM破裂出血,1例AVM位于运动区手术后症状加重,1例手术后2天并发迟发性静脉栓塞导致病情加重;2例患者死亡(12.5%),其中1例为AVM位于额叶运动区,在VS-SRS治疗后第6个月破裂再出血,虽经去骨瓣减压和AVM切除,仍死亡;另1例在VS-SRS后出现窦旁静脉狭窄和堵塞,导致严重的半球水肿,死亡。
表1. VS-SRS结合手术切除组与单纯VS-SRS高级别AVM患者的临床资料对比。
综上所述,VS-SRS可以降低AVM等级,从而致使高级别AVM转化为可手术切除的低级别AVM。因此,VS-SRS结合手术切除可以提高高级别AVM的治愈率,但该治疗方案的可行性和安全性有待大样本的多中心、前瞻性临床研究加以验证。
原始出处:
Abla AA, Rutledge WC, Seymour ZA, Guo D, Kim H, Gupta N, Sneed PK, Barani IJ, Larson D, McDermott MW, Lawton MT. A treatment paradigm for high-grade brain arteriovenous malformations: volume-staged radiosurgical downgrading followed by microsurgical resection. J Neurosurg. 2015 Feb;122(2):419-32. doi: 10.3171/2014.10.JNS1424
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言








#静脉#
23
好文值得点赞!继续关注学习。
60
#动静脉畸形#
31
进一步证实
63
#畸形#
25
#ROS#
23
不错的文章,多学习
137
不错的文章,多学习
155