J Urol:活检与根治性前列腺切除术之间的时间间隔影响治疗结果么?
2021-11-21 AlexYang MedSci原创
调查了活检与根治性前列腺切除术之间的时间间隔对治疗结果的影响情况。
前列腺癌(PC)存在惰性过程,明确良好的长期治疗结果所需的治疗时间表非常重要。对于低危疾病的男性来说,推迟治疗的安全性已被广泛接受。然而,人们对中度和高度风险男性PC的治疗推迟的影响还不太清楚。现有文献也受限于对短期结果(病理结果和生化复发)的依赖,并不能很好的展现出推迟与临床重要结果的关系,其中包括总生存。最近一项评估该问题的系统性综述中,包括的24项研究没有一项考虑到发展为去势抵抗性疾病,2项评估了转移情况,只有3项评估了总生存率。

关于延迟治疗对中/高危前列腺癌(PC)患者长期结果影响的数据有限。近期,来自美国的研究人员杂《J Urol》杂志上发表文章,调查了活检与根治性前列腺切除术之间的时间间隔对治疗结果的影响情况。
研究人员从1988年至2018年的SEARCH队列中,纳入了3962名接受前列腺根治术(RP)治疗的中/高危男性患者。Cox比例风险模型评估了从活检到RP(最长1年)的时间与去势抵抗性PC(CRPC)、转移和全因死亡时间之间的关联。交互作用项用来测试风险组的效应修正。
在3962名男性中,167人发展为CRPC,248人发生转移,884人在85个月的中位随访后死亡。活检和RP之间较长的延迟与CRPC风险的降低有关(调整后的HR=0.88,95%CI:0.80-0.98,p=0.02),且与D'Amico风险组无关(交互作用p>0.05)。在患有中度和高度危险疾病的男性中,研究人员发现与RP的间隔时间长度与转移发生的风险(分别为p=0.5和0.9)或全因死亡率(分别为p=0.1和0.1)之间没有统计学显著意义。
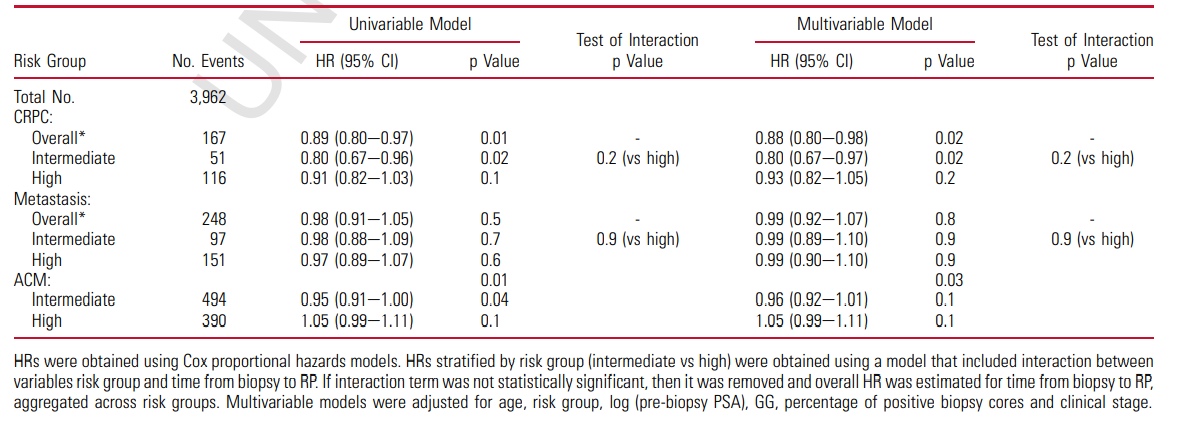
推迟时间与长期临床结果的风险比
综上所述,在中度和高度危险的男性PC患者中,PC诊断后,到RP治疗时间达1年的男性中,其不良的长期结果,包括CRPC、转移和死亡的风险均没有统计学显著意义的增加。
原始出处:
Maggie C Lee , Tyler R Erickson , Shannon Stock et al. Association Between Delay to Radical Prostatectomy and Clinically Meaningful Outcomes Among Patients with Intermediate- and High-Risk Localized Prostate Cancer. J Urol. Oct 2021
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言













#前列腺切除#
37
#切除术#
41
#活检#
39
#治疗结果#
53
#根治#
33