双瓣膜病变伴冠脉高险:江西省心血管病医院洪浪院长带领团队顺利完成1例一站式PBMV+TAVR冠脉高风险手术
2021-07-08 “Clinic門诊新视野”公众号 “Clinic門诊新视野”公众号
2021年6月29日,江西省心血管病医院洪浪院长带领团队完成1例一站式PBMV+TAVR冠脉高风险手术,在医院多学科协同下,手术取得圆满成功,患者苏醒后即刻拔管。术后第一天即下床并转回普通病房。
2021年6月29日,江西省心血管病医院洪浪院长带领团队完成1例一站式PBMV+TAVR冠脉高风险手术,在医院多学科协同下,手术取得圆满成功,患者苏醒后即刻拔管。术后第一天即下床并转回普通病房。
病况概述&术前评估
患者为70岁男性,主诉于1月前开始出现反复胸闷、气逼,常在活动或劳累时发生,每次持续数分钟至半小时不等,休息后可缓解,无头晕、心慌,无心悸、恶心呕吐,无咳嗽、咳痰等不适。为求进一步规范治疗,来我院治疗,门诊拟“风湿性心脏病”收治入科。起病以来,精神、食欲、睡眠尚可。大小便正常,体重无明显改变。
术前心超示:风湿性心脏病,主动脉瓣重度狭窄并中度关闭不全(平均跨瓣压差为90 mmHg、流速4.7 m/s、瓣口面积0.58 cm2);二尖瓣轻中度狭窄并中度关闭不全(瓣口面积1.2 cm2)升主动脉扩张;左室舒张末直径41 mm;EF 59%。
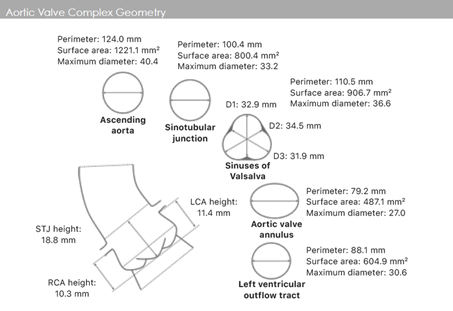
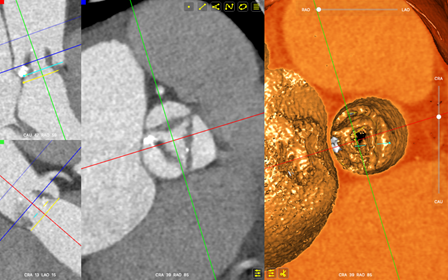
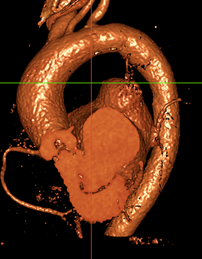
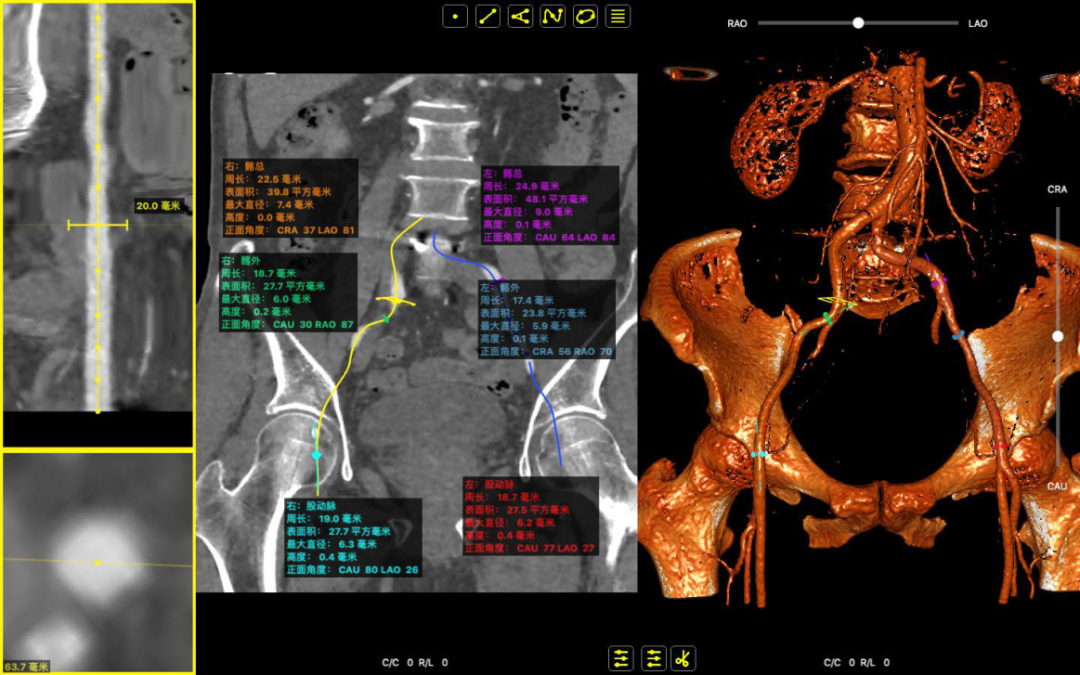
主动脉根部CT示:风湿性三叶瓣,瓣叶增厚约4 mm且左右右融合,钙化主要分布在无冠窦瓣叶,升主动脉扩张,双侧髂股动脉内径可;瓣环周长约79.2 mm(平均直径25.2 mm),环上瓣周长约69 mm(平均直径21.9 mm)左室流出道周长88.1 mm(平均直径28 mm),升主周长124 mm(瓣上40 mm)。左冠高度11.4 mm(瓣叶长约15 mm,左冠开口上缘高度在16 mm左右),右冠高度10.3 mm(瓣叶长约15.9 mm,左冠开口上缘高度在16.5 mm左右),窦宽31.9~34.5 mm。
缜密规划 &精准植入
术前,洪院长组织心内科、心外科、超声科、CCU病房、介入室等科室进行术前策略分析,考虑到患者双瓣膜病变,且呈现风湿性瓣叶增厚,右冠开口较低(右冠闭塞风险高)。经过多层面的讨论后,洪浪院长决定先行二尖瓣球囊成型术(PBMV),再处理主动脉瓣病变,如22 mm球扩影响冠脉血流,则预埋支架及延长导管做冠脉保护,24 VitaFlow(27备选)定位释放。
术中操作全流程:
冠脉造影
房间隔穿刺

二尖瓣球囊扩张
经左股动脉猪尾送至主动脉根部并造影(短径方向投射角度)
跨瓣操作
导丝引导下瓣膜输送至病变处

窦部造影确认瓣膜定位
释放后最终造影显示瓣膜位置良好,微量反流

术后即刻超声良好:平均压差:0 mmHg
为患者至专至精·以匠心诠释精益求精

该例病例的整体难点/特点在于:风湿性三叶瓣,重度狭窄,瓣叶增厚约4 mm;右窦瓣叶较长,且右冠开口低,冠脉高风险;PBMV+TAVR 一站式处理二尖瓣、主动脉瓣狭窄。患者的二尖瓣中度狭窄和主动脉瓣重度狭窄问题需要同时得到解决,而其CT评估结果又提示右冠高闭塞风险。所幸,洪浪院长带领的TAVR团队通过紧密配合、充分评估每个重要环节及其应对措施,为手术的成功奠定了良好基础。
术后,患者的平均跨瓣压差由术前的65 mmHg降至0 mmHg,仅少量瓣周漏。整个手术取得了圆满成功,患者苏醒后即刻拔管。术后第一天即下床并转回普通病房。相比传统开放手术,TAVR术式的优势更明显,无需开胸、心脏停跳及体外循环,手术时间短,失血少,麻醉时间短,微创恢复快。洪浪院长将继续与多学科协同作战,打造江西省心血管病医院一流的瓣膜诊疗团队,持续开展主动脉瓣及其二尖瓣等瓣膜介入手术,帮助更多患者恢复健康,享受高质量的晚年生活!
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言










#一站式#
39
#高风险手术#
29
#顺利完成#
36
#AVR#
33
#血管病#
32
#高风险#
34
#江西省#
33
#瓣膜#
35