J Periodontol:牙周炎患者心血管疾病和糖尿病相关药物的摄入率较高,且疾病严重程度与药物摄入率相关
2021-07-08 MedSci原创 MedSci原创
目前,关于牙周炎患者的用药情况以及与牙周健康状态的人相比是否有差异的信息有限。为此,研究人员调查了患有或不患有牙周炎的老年患者服用全身性药物的频率和类型,以及药物摄入频率与牙周炎严重程度之间可能存在的
目前,关于牙周炎患者的用药情况以及与牙周健康状态的人相比是否有差异的信息有限。为此,研究人员调查了患有或不患有牙周炎的老年患者服用全身性药物的频率和类型,以及药物摄入频率与牙周炎严重程度之间可能存在的联系,研究结果已发表于J Periodontol。
研究共纳入1221名患者,包括608名全身中重度牙周炎患者(牙周炎组)和613名年龄和性别匹配的牙周健康者(健康组)。记录了全身情况、药物和牙周状况。使用非条件逻辑回归法比较了药物摄入频率(%)。
结果显示,最常见的前三种药物是血管紧张素转换酶(ACE)抑制剂(17.9%)、抗抑郁药(17.8%)和降脂药物(16.5%)。相对于健康对照组,牙周炎组的ACE抑制剂(21.5% vs. 14.4%;OR =1.64)和抗抑郁药(21.1% vs. 14.5%,OR=1.57)的摄入频率明显更高(P <0.01)。此外,口服降糖药、钙通道阻滞剂(CCB)、胰岛素和利尿剂的摄入量在牙周炎组明显较高,OR=2.49、2.32、2.08和1.79(P <0.05)。几种药物与疾病严重程度有关,将全身重度牙周炎与中度牙周炎和健康组进行比较:口服降糖药(17.4% vs. 16.8% vs. 8.0%)、CCB(14.8% vs. 14.4% vs. 8.0%)和抗惊厥药(13.4% vs. 7.7% vs. 6.4%),OR分别为2.43、1.99和2.28(重度牙周炎与健康组)。
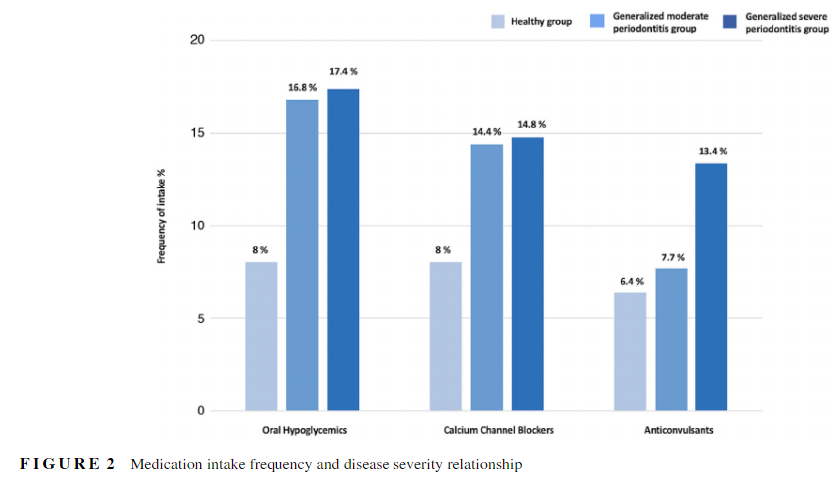
综上,在牙周炎患者中,与心血管疾病和糖尿病有关的药物摄入率明显更高,且疾病严重程度与药物摄入率存在相关关系。这项研究为系统性疾病和牙周炎之间可能存在的关系提供了间接证据。
原始出处:
I-Ching Wang, et al., Association between periodontitis and systemic medication intake: A case-control study. J Periodontol. 2020 Oct;91(10):1245-1255. doi: 10.1002/JPER.19-0593.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言














#PE#
37
#牙周#
39
#血管疾病#
33
厉害
67
学习了
77
很好
78
谢谢MedSci提供最新的资讯
63
好
62