Radiology:CT+CA19-9的强强联手:非转移性胰腺癌的治疗反应评估
2022-08-12 shaosai MedSci原创
总所周知,准确评估治疗反应对于癌症患者的管理非常重要。目前对大多数类型的肿瘤进行反应评估的标准方法是实体瘤反应评估标关于胰腺导管腺癌(PDAC),CT一直是治疗反应评估的主要依据。
总所周知,准确评估治疗反应对于癌症患者的管理非常重要。目前对大多数类型的肿瘤进行反应评估的标准方法是实体瘤反应评估标准(RECIST)1.1版,它包括四个类别:完全缓解、部分反应(PR)、疾病稳定(SD)和疾病进展(PD)。然而,RECIST并不总是作为患者生存的替代标记物的最佳选择,特别是对于特定类型的肿瘤或治疗方式来说更是如此。
关于胰腺导管腺癌(PDAC),CT一直是治疗反应评估的主要依据。然而,许多作者指出,影像学评价经常低估实际的治疗反应。相比之下,一线治疗期间碳水化合物抗原19-9(CA 19-9)水平变化的预测作用已被多项研究报道。最新的国家综合癌症网络指南(1.2021版)建议在评估PDAC患者的治疗反应时应综合影像学检查和CA 19-9水平共同评估。然而,整合这两个不同的参数--影像学研究结果(CT反应)和CA 19-9水平(CA 19-9反应)的最佳方法和临床意义在文献中没有得到很好的确立。
近日,发表Radiology杂志的一项研究探讨了在一线治疗开始后8周,CT(CT反应)和CA 19-9反应的联合评估对预测非转移性PDAC患者的总生存期(OS)的有效性。
本研究在2013年1月至2016年12月期间对一个单中心PDAC队列登记处接受化疗或同期化放疗一线治疗的非转移性PDAC患者回顾性地纳入了研究。根据实体瘤的反应评估标准,对治疗后8周获得的后续CT图像进行了评估。部分反应(PR)或疾病稳定(SD)的患者被定义为CT反应者,而疾病进展(PD)的患者被定义为CT无反应者。随访8周时CA 19-9水平恢复正常的患者被定义为CA 19-9应答者,而CA 19-9水平未恢复正常或未升高的患者被定义为CA 19-9无应答者。使用Kaplan-Meier方法和Breslow分析比较了OS。
共评估了197名患者(平均年龄±标准差,65岁±10;107名男性)。PD患者(n = 17)的OS比SD(n = 147;P < .001)或PR(n = 33;P = .003)的患者短。PR患者和SD患者的OS没有差异(P = .60)。当联合CT和CA 19-9反应时,CT和CA 19-9反应者的OS最长(第一组,n = 27;中位OS,26.6个月[95% CI: 9.0, 44.1]),其次是CT反应者但CA 19-9无反应者(第二组,n = 153;中位OS,15. 9个月[95% CI: 13.3, 18.5]; P = .007 vs 第一组)和CT及CA 19-9无反应者(第三组,n = 17; 中位OS,6.5个月[95% CI: 0.8, 12.2]; P < .001 vs 第二组)。
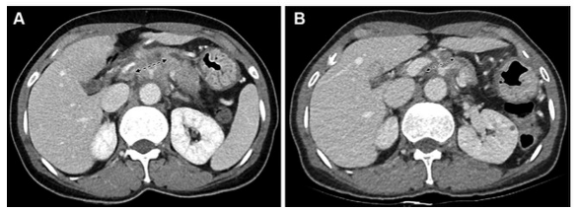
图 一名54岁胰腺导管腺癌患者的图像,为第一组的代表性病例(CT和CA 19-9反应者)。(A) 基线对比增强CT图像显示胰腺体部有一个30毫米的肿块,腹腔动脉和肝总动脉被包围(箭头)。该肿块为局部晚期可切除状态。基线CA 19-9水平为391.9 U/ml。(B)使用5-氟尿嘧啶、亮丙瑞林、伊立替康和奥沙利铂或FOLFIRINOX一线治疗8周后获得的后续对比增强CT图像。由于肿块的大小略微下降到27毫米(箭头),根据实体瘤的反应评价标准,治疗反应被归类为疾病稳定(CT反应者)。由于CA 19-9水平也降至29.2 U/mL,低于37 U/mL的临界值,患者被归类为CA 19-9反应者。没有进行手术切除。在获取数据时,该患者还存活,总生存期为44.7个月
本研究表明,本研究对CT和CA 19-9反应的综合评价在日常临床实践中易于应用,与实体瘤的反应评价标准相比,能更准确地对非转移性胰腺腺癌患者在治疗早期的生存状况进行分层。按生存率降序排列,各组可分为:第1组(CT和CA 19-9反应者)、第2组(CT反应者但CA 19-9无反应者)及第3组(CT和CA 19-9无反应者)。无论可切除性状况如何,CT和CA 19-9反应者均可成为手术探查的潜在候选人。
原文出处:
Seung-Seob Kim,Sunyoung Lee,Hee Seung Lee,et al.Retrospective Evaluation of Treatment Response in Patients with Nonmetastatic Pancreatic Cancer Using CT and CA 19-9.DOI:10.1148/radiol.212236
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











#非转移性#
51
#非转移#
44
#转移性#
39
#转移性胰腺癌#
52