Blood:代替多位点骨穿活检确定风险风采的新方法——局部病损大小数量指示风险风层
2018-05-22 MedSci MedSci原创
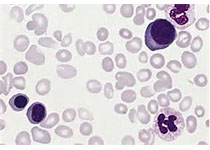
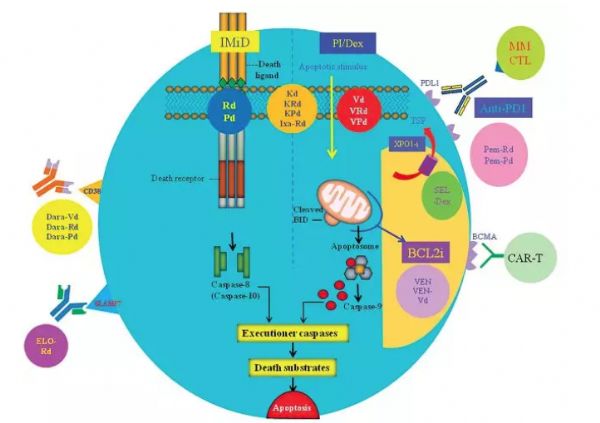
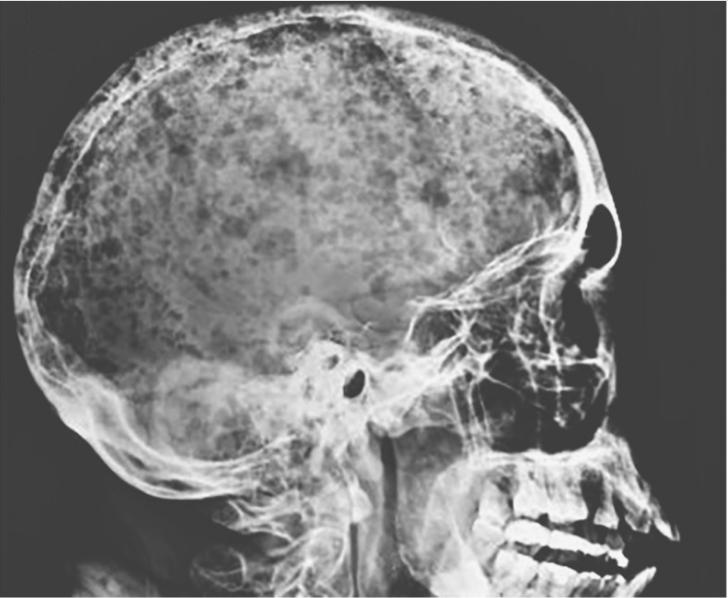
中心点:对于新确诊的骨髓瘤患者,存在≥3个大面积局部病损,预后不良。多发大面积局部病损的预测意义独立于R-ISS、GEP70和髓外疾病之外。摘要:在多发性骨髓瘤(MM)中常可见到空间内部肿瘤异质性,这对依赖于髂嵴穿刺的肿瘤样本的风险分层来说是一个巨大挑战。鉴于对多个骨骼部位进行活检评估比较困难,我们需要可代替的风险分层方法。近日发现,局部病损(FL)的大小似乎可作为空间异质性的替代标志物,提示医学
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言










#新方法#
25
#活检#
31
#局部#
29
学习了.谢谢分享
63
学习
49
一起学习学习
71