Cancer Cell:张泽民团队等揭示抗PD-L1免疫治疗联合化疗在三阴性乳腺癌中的作用机制
2021-10-18 “E药世界”公众号 “E药世界”公众号
2021年10月14日,北京大学生物医学前沿创新中心(BIOPIC)张泽民课题组联合中国医学科学院肿瘤医院刘芝华课题组、马飞和徐兵河课题组,在肿瘤学顶级期刊 Cancer Cell 上在线发表了题为
乳腺癌位于女性恶性肿瘤之首,其中三阴性乳腺癌(Triple-Negative Breast Cancer,TNBC)是复发率和死亡率最高的乳腺癌亚型。三阴性乳腺癌对激素疗法和靶向疗法均无效,目前以传统化疗为主要治疗手段,但效果不甚理想。
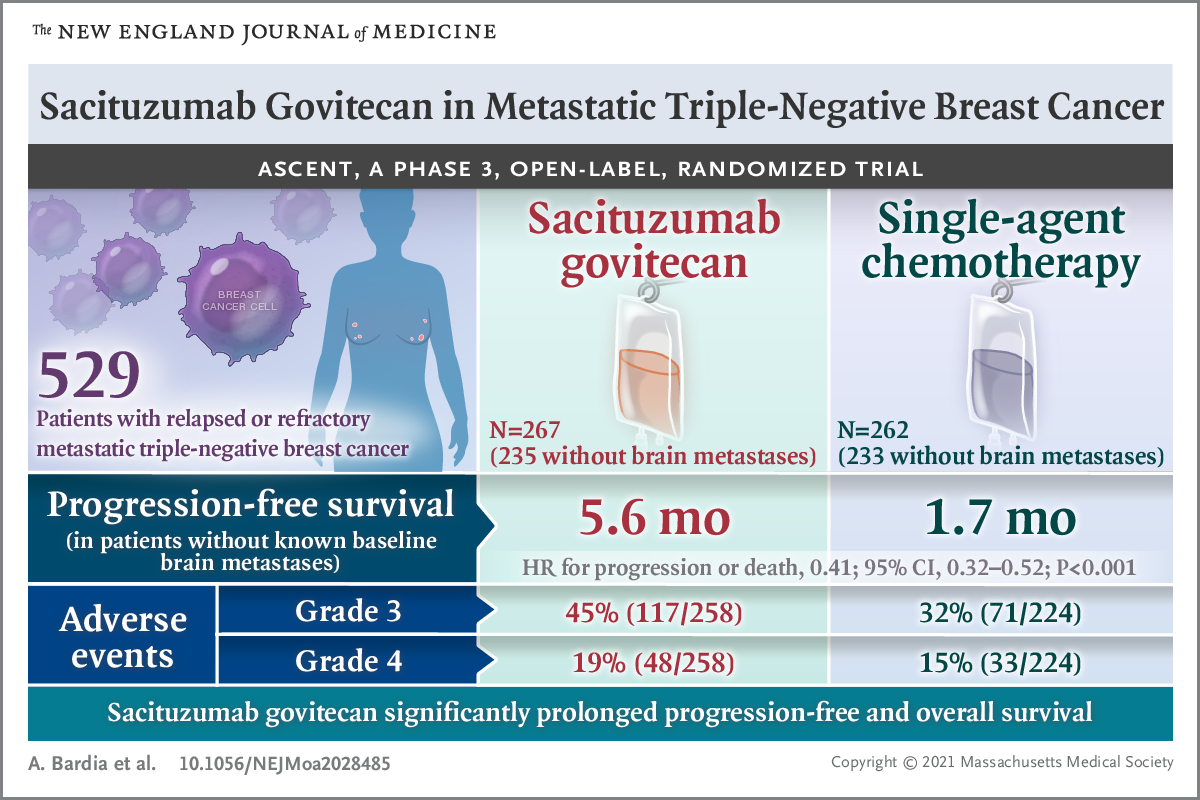
尽管癌症免疫治疗已进入快速发展时期,三阴性乳腺癌的免疫治疗却举步维艰: 虽然早期IMpassion 130临床试验表明,anti-PD-L1抗体阿替利珠单抗(Atezolizumab)联合白蛋白结合型紫杉醇(Nab-paclitaxel)能够显着降低PD-L1+阴性乳腺癌患者的无疾病进展或死亡风险,然而近期IMpassion 131临床试验表明,阿替利珠单抗联合紫杉醇却无法使三阴性乳腺癌患者获益。
不同临床试验的结果差异提示不同的化疗药物可能会导致不同的肿瘤微环境特征,进而影响免疫检查点抑制剂的治疗效果。系统解析用药前后的肿瘤微环境变化是理解当前免疫治疗和化疗药物的作用机制、以及提高三阴性乳腺癌整体治疗效果的关键。
2021年10月14日,北京大学生物医学前沿创新中心(BIOPIC)张泽民课题组联合中国医学科学院肿瘤医院刘芝华课题组、马飞和徐兵河课题组,在肿瘤学顶级期刊 Cancer Cell 上在线发表了题为:Single-cell analyses reveal key immune cell subsets associated with response to PD-L1 blockade in triple negative breast cancer 的研究论文。
研究人员收集了来自22例三阴性乳腺癌患者(11例接受阿替利珠单抗联合紫杉醇化疗,11例接受紫杉醇单药化疗)治疗前和治疗后的78例配对样本,通过整合单细胞转录组测序、T细胞受体序列测序和染色质可及性测序,构建了三阴性乳腺癌患者肿瘤微环境和外周血来源免疫细胞的高分辨率转录组和表观组动态图谱。
该研究在单细胞水平上对来自接受两种治疗方案的三阴性乳腺癌病人的肿瘤组织和外周血的免疫细胞进行刻画,系统比较了响应患者和非响应患者的肿瘤微环境及外周血免疫特征,阐明了免疫细胞在不同治疗方案下的动态变化,揭示了anti-PD-L1免疫治疗联合紫杉醇化疗在三阴性乳腺癌中的作用机制。
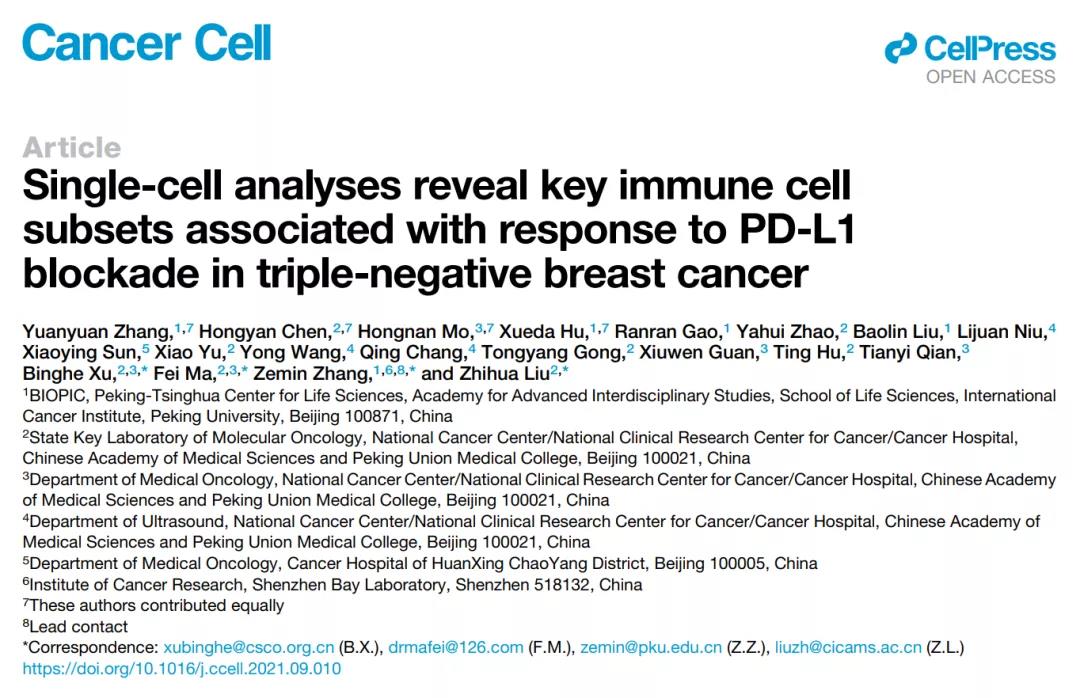
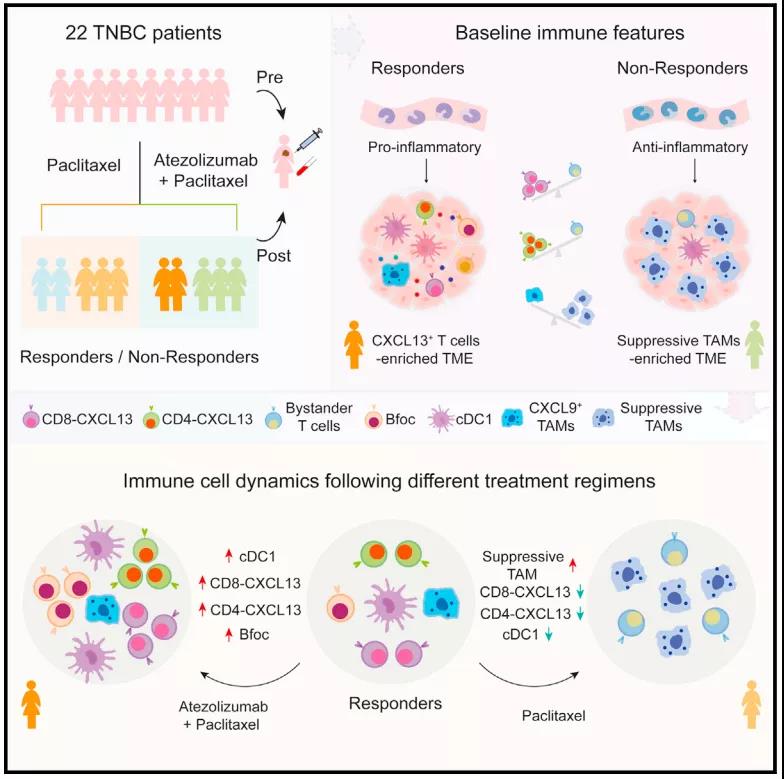
图 1 课题研究方案及主要结论
通过比较联合用药组不同响应患者的肿瘤及外周血免疫细胞的组成差异,研究人员发现响应患者的肿瘤微环境富集了两群高表达CXCL13的T细胞(CD8-CXCL13和CD4-CXCL13),这两群细胞同时高表达T细胞毒性和“耗竭”相关基因。为了进一步精确刻画不同免疫细胞的组成成分和比例变化与治疗效果的关联,研究人员设计了两个指数:“预测指数”和“治疗指数”,通过“预测指数”和“治疗指数”分析,研究人员发现更高基线水平的CD8-CXCL13和CD4-CXCL13能够预测更好的免疫治疗响应,且这两群CXCL13+ T细胞在响应患者中经过联合用药后细胞比例显着增加。
此外,研究人员发现响应患者的肿瘤微环境中富集了两群高表达CXCL9和CXCL10的促炎性巨噬细胞,且这两群促炎性巨噬细胞与CXCL13+T细胞存在显着正相关。CXCL9和CXCL10能够参与T细胞招募,而促炎性巨噬细胞的特征基因受到IFNG和TNF信号调控,表明发挥杀伤功能的CXCL13+T细胞与高表达CXCL9和CXCL10的促炎性巨噬细胞之间存在正反馈信号。与之相反,不响应患者的肿瘤微环境中几乎检测不到CXCL13+T细胞,但富集了大量发挥免疫抑制功能的巨噬细胞。值得注意的是,研究人员发现响应患者的外周血单核细胞表现出促炎特征,而不响应患者的外周血单核细胞表现出抗炎特征,提示外周血能够在一定程度上反应肿瘤微环境特征。
肿瘤微环境是一个复杂的生态系统,其中固有免疫和适应性免疫细胞、基质细胞、癌细胞及其相互作用,构成精细的调节网络,共同决定癌症的发生和发展。虽然T细胞是当前肿瘤免疫研究的重点细胞类型,其他类型的免疫细胞亦可通过调控作用或与T细胞互作,影响免疫治疗效果。
通过系统刻画免疫细胞的比例组成及动态变化,研究人员发现B细胞尤其是滤泡B细胞,显着富集在响应患者的肿瘤微环境中,且其在免疫治疗后显着增加。进一步通过相关性分析及配体-受体互作对共表达分析,研究人员发现滤泡B细胞与CXCL13+T细胞显着正相关且存在相互作用。
此外,基于单细胞水平的细胞组成和TCGA公共数据的特征基因表达,研究人员发现cDC1与CXCL13+T细胞显着正相关,且cDC1在免疫治疗作用下显着增加,暗示cDC1可能参与CXCL13+T细胞的激活。通过比较化疗组和联合用药组免疫细胞的动态变化,研究人员发现与联合用药相反,紫杉醇单药化疗方案能够显着降低响应患者肿瘤微环境中的CXCL13+T细胞,并导致具有免疫抑制功能的巨噬细胞在肿瘤微环境中富集。
上述发现表明,紫杉醇化疗方案可能会削弱核心抗肿瘤免疫细胞,而免疫检查点抑制剂则能够显着增加核心抗肿瘤免疫细胞,提示紫杉醇化疗方案与阿替利珠单抗联合应用时,会影响anti-PD-L1抗体对三阴性乳腺癌患者的治疗效果。
综上,该研究揭示了三阴性乳腺癌患者对于anti-PD-L1免疫治疗敏感和耐药的分子机制,鉴定了关键免疫组分及其在免疫检查点抑制剂和紫杉醇化疗方案下的动态变化,阐明了紫杉醇化疗与阿替利珠单抗联合应用不能有效增加三阴性乳腺癌患者治疗效果的原因。该课题的研究结果对于当前免疫治疗联合化疗方案有重要指导意义,提示需要进一步系统评估不同化疗药与免疫治疗药联合使用的分子机制,才能有效提高联合用药方案对三阴性乳腺癌患者的治疗效果。
此项国际领先的新颖性工作,是迄今为止针对三阴性乳腺癌肿瘤相关免疫细胞的规模最大的单细胞组学研究,为深入理解三阴性乳腺癌患者的免疫特质及免疫治疗联合化疗方案的作用机制提供了可靠基础,也为后续相关研究工作提供了极有价值的数据资源。该研究的科学发现为解析肿瘤及其他疾病中免疫细胞的动态调控、指导三阴性乳腺癌患者临床分型以实现精准治疗、以及开发新的临床检测与治疗手段提供了新的思路。
北大-清华生命科学联合中心(CLS)博士后张园园博士,中国医学科学院肿瘤医院陈洪岩博士、莫红楠博士,及百奥智汇胡学达博士为该论文的并列第一作者。北京大学BIOPIC张泽民教授,中国医学科学院肿瘤医院刘芝华教授、马飞教授和徐兵河教授为该论文的共同通讯作者。该研究得到北京市科委、国家自然科学基金、国家重点研发计划、ICG的支持和资助。张园园博士得到北京大学博雅博士后及拜耳博士后基金的资助。
原始出处:
Yuanyuan Zhang, et al. Single-cell analyses reveal key immune cell subsets associated with response to PD-L1 blockade in triple-negative breast cancer. Cancer Cell,2021.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#Cell#
26
#CEL#
0
#cancer cell#
38
#阴性乳腺癌#
36
#PD-L1#
34
#联合化疗#
35
#三阴性#
50