Clin Respir J:根据细胞因子可以辨别社区获得性肺炎的感染原因
2020-07-28 MedSci原创 MedSci原创
社区获得性肺炎(CAP)可能不必要地使用抗生素,导致抗生素耐药病原体的选择。治疗开始时的细胞因子表达可能有助于识别不需要抗生素的患者。我们确定了回顾性分类为严格的病毒性、肺炎球菌性或病毒-细菌联合CA
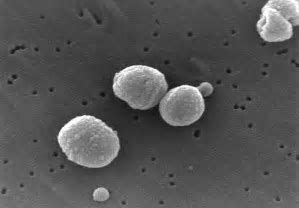
社区获得性肺炎(CAP)可能不必要地使用抗生素,导致抗生素耐药病原体的选择。治疗开始时的细胞因子表达可能有助于识别不需要抗生素的患者。我们确定了回顾性分类为严格的病毒性、肺炎球菌性或病毒-细菌联合CAP的患者的血浆细胞因子模式。本研究旨在探讨基于细胞因子的预测模型是否可以用于区分入院时的严格病毒性CAP和其他病因。
从344名住院的CAP患者中,104名患者被分为病毒性CAP(n = 17)、肺炎球菌CAP(n = 48)和细菌-病毒联合CAP(n = 39)。入院时测定血浆中IL-6、IL-10、IL-27、IFN-γ和C反应蛋白(CRP)。使用两个多变量回归模型和ROC曲线探讨了严格的病毒病因预测。
结果显示,使用多种细胞因子水平(IL-6、IL-27和CRP)通过logistic回归预测病毒性肺炎,AUC为0.911(95% CI:0.852-0.971,P <.001)。对于同样的患者,CRP的AUC为0.813(95% CI:0.728-0.898,P < .001)。
综上所述,该研究表明,在选定的CAP患者中,细胞因子的表达在病毒和细菌病因之间存在差异。有必要进行前瞻性验证研究。
原始出处:
Eduard H Burgmeijer, Ruud Duijkers, et al., Plasma cytokine profile on admission related to aetiology in community-acquired pneumonia. Clin Respir J. 2019 Oct;13(10):605-613. doi: 10.1111/crj.13062.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言













#获得性#
38
#胞因子#
26
#细胞因子#
31
#社区#
33
#学习#
106