GUT: 质子泵抑制剂的使用可能会增加胃癌的发生率
2021-05-22 MedSci原创 MedSci原创
胃癌是全世界第六大最常见的癌症,癌症相关死亡率则排第三位,慢性幽门螺杆菌感染是胃癌的最强危险因素。根除幽门螺杆菌可减少胃癌的发生。
胃癌是全世界第六大最常见的癌症,癌症相关死亡率则排第三位,慢性幽门螺杆菌感染是胃癌的最强危险因素。根除幽门螺杆菌可减少胃癌的发生。但是,根除幽门螺杆菌并没有完全预防胃癌的发生。质子泵抑制剂(PPI)是作用于胃H+/K+ATPase的抑制剂并已被用于消化性疾病的治疗。长期使用PPI可能会增加患胃病的风险,即使在根除幽门螺杆菌后仍会罹患癌症。因此,本项研究旨在评估PPI使用与胃癌之间的关系。

研究人员分析了2002年至2013年间韩国国家健康保险服务数据库的原始数据,对所有接受一年PPI治疗的患者均进行了回顾性研究,通过Cox比例风险模型比较了PPI与其他药物之间胃癌的发生率,最后还分析了幽门螺杆菌根除后PPI使用者中胃癌的发生率。
本项研究共纳入了11741例接受PPI治疗和非PPI治疗的患者。在4.3年的中位随访期间,使用PPI与胃癌发生率增加2.37倍相关(HR 2.37,95%CI 1.56-3.68,p = 0.001)。胃癌的发病也与PPI的使用时间有关。在幽门螺杆菌根除的受试者中,与非PPI组相比,胃癌的发生率与180天以上的PPI使用显着相关( HR 2.22,95%CI 1.05至4.67,p = 0.036)。
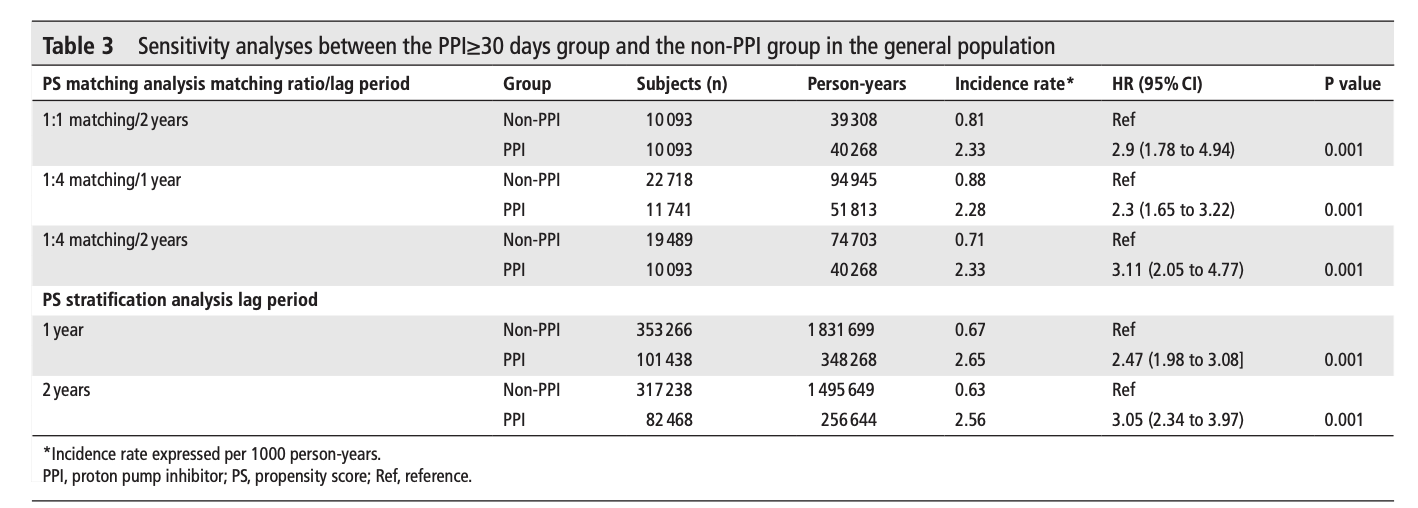
图:PPI对于胃癌的影响
本项研究证实PPI的使用与胃癌的发生率有关,而与幽门螺杆菌的根除状态无关。在胃癌高风险地区应谨慎长期使用PPI。
原始出处:
Seung In Seo. Et al. Association between proton pump inhibitor use and gastric cancer: a population-based cohort study using two different types of nationwide databases in Korea. GUT.2021.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#抑制剂#
49
学习的
68
#发生率#
36
#质子泵#
54