Lancet子刊:西安交大:中老年人肌肉减少或导致心血管疾病风险激增!
2022-01-20 MedSci原创 MedSci原创
肌少症可能与中国中老年人的高心血管疾病风险有关。
肌肉减少症是一种严重的老年综合症,表现为骨骼肌肉质量下降,加上肌肉力量低下,及/或体能低下,是老龄化社会面临的公共卫生问题。在过去十年,多项研究报告指出,在亚洲地区的老年人中,"肌肉减少症 "的发病率由6.8%至25.7%不等。
年龄的增长是与心血管疾病(CVD)发展相关的最强风险因素,是老年患者死亡的主要原因之一。最近,越来越多的研究探讨了肌少症与CVD之间的关系,如冠心病、心房颤动、心力衰竭和中风。
目前对中国人群中老年人肌少症与CVD之间的关系知之甚少。为此,来自西安交大附属医院的专家利用中国健康与退休纵向研究(CHARLS)中具有全国代表性的数据,进行了横断面和纵向分析,以研究中国中老年人群中肌肉疏松症状态与心血管疾病之间的关系。结果发表在《柳叶刀》子刊EclinicalMedicine杂志上。
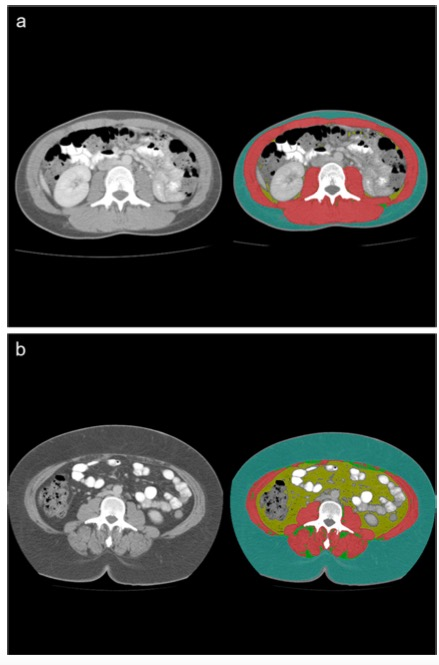
该样本包括15137名年龄在45岁以上的CHARLS 2015的参与者。肌少症状态是根据2019年亚洲肌少症工作组(AWGS 2019)的标准来定义的。CVD为存在医生诊断的心脏病和/或中风。从CHARLS 2015中共招募了11863名无CVD的参与者,并在2018年进行了随访。进行了Cox比例危害回归模型,研究了肌少症对心血管的影响。
在总体人群中,无肌少症、可能的肌少症和肌少症患者的CVD患病率分别为12.6%(1905/15137)、10.0%(1026/10280)、18.1%(668/3685)、18.0%(211/1172)。在总人群中,可能的肌少症[OR(95%CI):1.29(1.13-1.48)]和肌肉疏松症[1.72(1.40-2.10)]分别与CVD风险增加29%和72%有关。

2015-2018年,基线肌少症状态与新发生CVD的纵向关联。
在3.6年的随访中,确定了1273例(10.7%)发生CVD的病例。在纵向分析中,被诊断为可能患有肌少症的人(HR=1.22,95% CI:1.05-1.43)和肌少参与者(HR:1.33,95% CI:1.04-1.71)比没有肌少症的同龄人新发CVD的风险增加22%与33%。
综上,使用2019年AWGS标准评估的"肌少症 "可能与中国中老年人的高心血管疾病风险有关。
参考文献:
Association between sarcopenia and cardiovascular disease among middle-aged and older adults: Findings from the China health and retirement longitudinal study. DOI:https://doi.org/10.1016/j.eclinm.2021.101264
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言

















#中老年#
33
#Lancet#
23
#西安交大#
28
#中老年人#
35
#肌肉减少#
29
#激增#
21
#疾病风险#
23
#血管疾病#
24