CTM:用列线图预测结直肠癌患者特定位点远处转移和总体生存大规模人群研究
2020-05-17 程欣 CTMWorld
在美国仅2019年就有148000名新结直肠癌(CRC)患者,其中每天有146名患者死亡,占所有恶性肿瘤死亡率的第三位。在过去的30年间,CRC在全世界范围内的发病率和总体生存率(OS)一直在升高。5
在美国仅2019年就有148000名新结直肠癌(CRC)患者,其中每天有146名患者死亡,占所有恶性肿瘤死亡率的第三位。在过去的30年间,CRC在全世界范围内的发病率和总体生存率(OS)一直在升高。5年CRC的OS大约是65.2%。影响CRC生存率的主要原因是远处转移,包括肝,肺,脑和骨转移。
2020年4月29日,Clinical and Translational Medicine杂志在线发表了复旦大学彭俊杰教授团队的最新成果 “ Nomograms for predicting specific distant metastatic sites and overall survival of colorectal cancer patients: A large population-based real-world study”[6]
本项研究的目的是制作可以预测CRC患者特定位点远处转移和总体生存的功能性列线图。作者根据已有的公共数据库对CRC病例进行了大规模的回顾性研究。然后制作了可以预测CRC患者特定位点远处转移可能性和总体生存的列线图。用C-index,校正曲线,曲线下面积(AUC),决策曲线(DCA)等指标评估列线图的功能效果。

在本项研究中共收集了142343个病例。单变量和多变量分析结果表明, 某些临床病理特征与特定位点远处转移和生存情况相关,据此制作了列线图。结果表明制作的列线图可以十分精确地预测特定远处转移位点。预测肝,肺,骨和脑转移的C-index分别为0.82(95%可信区间(CI),0.81-0.83),0.80(95%CI,0.78-0.81),0.83(95%CI,0.79-0.86)和0.73(95%CI,0.72-0.84)。然后绘制了可以预测CRC患者1年,3年,5年OS的预后列线图,此列线图综合了CRC临床病理特征和特定远处转移位点,得出的AUCs分别为0.764(95%CI,0.741-0.783),0.762(95%CI,0.745-0.781)和0.745(95%CI,0.730-0.761)。DCA表明预后列线图的临床应用价值要好于目前的TNM分期系统。
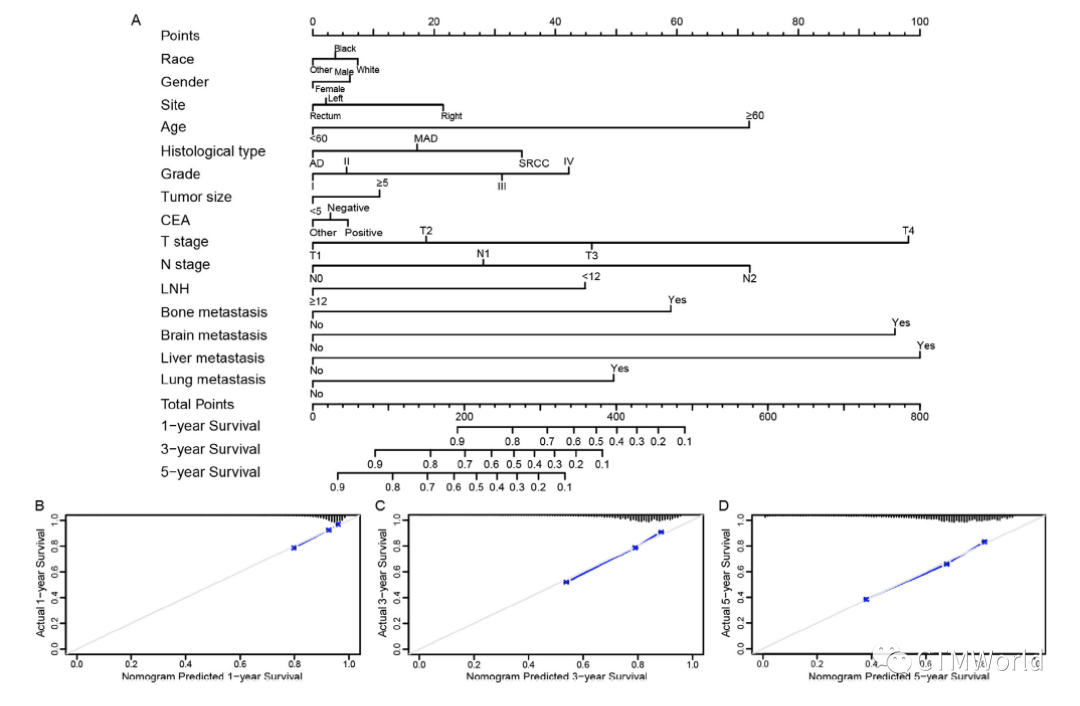
结论是根据临床病理特征为临床医生构建的列线图可以预测CRC患者特定远处转移位点和OS。这有助于对手术后CRC患者进行个体化评估。
总之,作者为CRC患者绘制了全新的可以预测特定远处转移位点和OS的列线图。这种简单清晰的列线图不仅有很好的临床应用价值,而且还有足够的区分和校准功能。这有助于临床医生评价每位CRC患者的预后和制定个体化的治疗方案。
彭俊杰
彭俊杰,男,复旦大学附属肿瘤医院大肠外科副主任医师。毕业于复旦大学临床医学系,2009年毕业于复旦大学附属肿瘤医院肿瘤学博士。曾在美国加州大学旧金山分校(UCSF)肿瘤中心从事临床博士后研究。自2006年起,一直在复旦大学附属肿瘤医院大肠外科工作,曾任住院医生, 主治医生。目前担任中国抗癌协会大肠癌专业委员会肝转移学组委员、中国医师协会外科分会结直肠癌专业委员会青年委员、中国医师协会外科分会多学科协作组委员会青年委员、中国家族遗传性协作组结直肠癌分组委员。主要擅长结直肠癌的根治性手术、微创手术及多学科综合治疗,在遗传性大肠癌、结直肠癌肝转移及晚期结直肠癌的化疗敏感性方面有深入研究。
REFERENCES
1. Siegel RL,Miller KD, Jemal A. Cancer statistics, 2020. CA Cancer J Clin. 2020;70(1):7-30.
2. Zhou Z, Mo S, Dai W, et al. Prognostic nomograms for predicting cause-specific survival and overall survival of stage I-III colon cancer patients: a large population-based study. Cancer Cell Int. 2019;19:355.
3. O’Connell JB, Maggard MA, Ko CY. Colon cancer survival rates with the new American Joint Committee on Cancer sixth edition staging. J Natl Cancer Inst. 2004;96(19):1420-1425.
4. Zhou Z, Mo S, Dai W, et al. Development and validation of an autophagy score signature for the prediction of post-operative survival in colorectal cancer. Front Oncol. 2019;9:878.
5. Gryfe R, Kim H, Hsieh ET, et al. Tumor microsatellite instability and clinical outcome in young patients with colorectal cancer. N Engl J Med. 2000;342(2):69 77.
6. Mo S, Cai X, Zhou Z, et al. Nomograms for predicting specific distant metastatic sites and overall survival of colorectal cancer patients: A large population-based real-world study. Clin Transl Med . 2020;10:169–181.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#大规模#
37
#列线图#
49
不错
104
#远处转移#
44
#结直肠#
30
很好的学习机会
95
会各种统计方法也是有优势的
98
列线图只是方法而已
104