JCO:ACHIEVE研究最终结果:III期结肠癌奥沙利铂为基础化疗辅助治疗3个月对比6个月的疗效和安全性
2022-05-23 yd2015 网络
在亚洲III期结肠癌患者中,将辅助治疗时间从6个月缩短到3个月并不影响疗效,并降低了长期外周感觉神经病变的发生率。在这种情况下,3个月的CAPOX治疗是一个合适的辅助治疗选择。
在日本进行的III期ACHIEVE试验是IDEA研究中包括的6项前瞻性研究之一,该研究主要是探讨在根治性切除的III期结肠癌患者中,3个月的FOLFOX或CAPOX方案辅助化疗是否非劣效于6个月的疗效。近期,Journal of Clinical Oncology杂志上发表了其最终的生存结果和长期安全性结果。
符合条件的患者被随机(1:1)分配到3个月或6个月的辅助化疗(由治疗医生选择改良的FOLFOX6或CAPOX)。根据受累淋巴结数量、中心、治疗方案、原发部位和年龄进行随机分层。主要终点为无病生存期,在改良意向治疗人群中进行评估。总生存期(OS)是次要终点。
改良治疗意向人群包括1,291名患者:6个月治疗组641名,3个月治疗组650名。本次分析的中位随访时间为74.7个月。3个月治疗组的5年DFS率为75.2% (95% CI, 71.7 - 78.4), 6个月治疗组的5年DFS率为74.2% (95% CI, 70.6 - 77.5) (HR, 0.95;95% CI, 0.77 ~ 1.18;P=0.64)。对于接受mFOLFOX6治疗的患者,3个月治疗组的5年DFS率为68.6% (95% CI, 60.8 - 75.1), 6个月治疗组的5年DFS率为69.7% (95% CI, 61.8 - 76.2) (HR, 1.04;95% CI, 0.71 ~ 1.54;P=0.82);对于接受CAPOX的患者,3个月治疗组的5年DFS率为77.4% (95% CI, 73.4 ~ 80.9), 6个月治疗组的5年DFS率为75.8% (95% CI, 71.6 ~ 79.4) (HR, 0.91;95% CI, 0.71 ~ 1.18;P=0.49)。

对于低危患者,3个月治疗组的5年DFS率为86.5% (95% CI, 82.5 - 89.7), 6个月治疗组的5年DFS率为84.8% (95% CI, 80.6 - 88.2) (HR, 0.85;95% CI, 0.59 ~ 1.23;P=0.39);对于高危患者,3个月治疗组5年DFS率为60.7% (95% CI, 54.8 ~ 66.2), 6个月治疗组5年DFS率为61.5% (95% CI, 55.6 ~ 66.9) (HR, 1.04;95% CI, 0.80 ~ 1.35;P=0.75)。
根据风险组和治疗方案进行DFS分析,低危患者中,3个月mFOLFOX6治疗可能比6个月mFOLFOX6治疗的预后更差(HR, 1.41;95% CI, 0.68 ~ 2.91;P=0.35)。相反,3个月的CAPOX治疗似乎优于6个月的CAPOX治疗(HR, 0.70;95% CI, 0.45 ~ 1.09;P=0.11)。对于高危患者,mFOLFOX6(HR, 1.01;95% CI, 0.63 ~ 1.60;P=0.98)和CAPOX (HR, 1.07;95% CI, 0.78 ~ 1.46;P=0.70)治疗3个月和6个月的结果相似。
3个月治疗组的5年OS率为87.0% (95% CI, 84.2 - 89.4), 6个月治疗组的5年OS率为86.4% (95% CI, 83.5 - 88.9) (HR, 0.91;95% CI, 0.69 ~ 1.20;P=0.51)。对于接受mFOLFOX6治疗的患者,3个月治疗组的5年OS率为83.2% (95% CI, 76.5 - 88.2), 6个月治疗组的5年OS率为84.6% (95% CI, 77.9 - 89.4) (HR, 0.99;95% CI, 0.61 ~ 1.60;P=0.95),对于接受CAPOX的患者,3个月治疗组的5年OS率为88.3% (95% CI, 85.1 - 90.9), 6个月治疗组的87.0% (95% CI, 83.6 - 89.7) (HR, 0.87;95% CI, 0.62 ~ 1.22;P=0.42)。
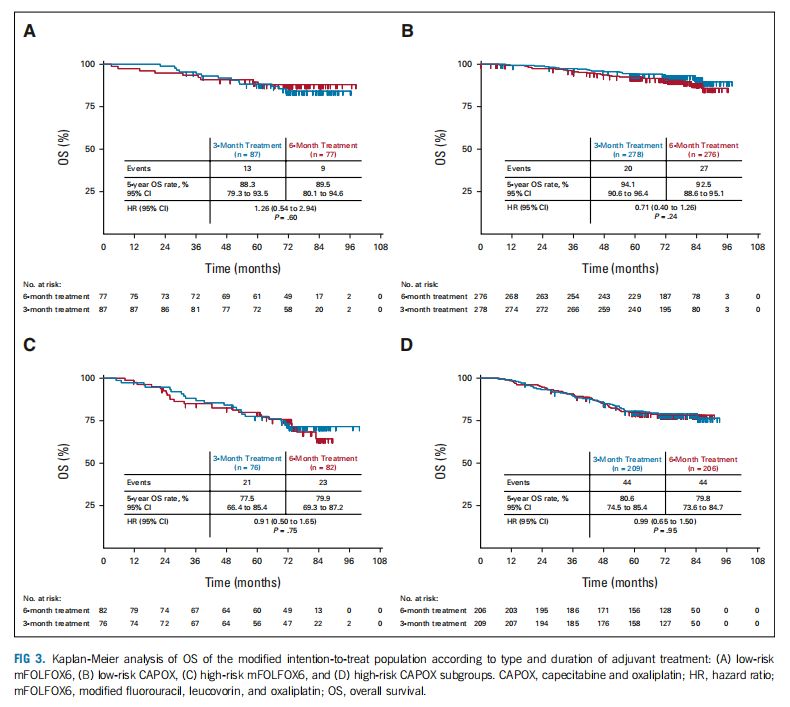
对于低危患者,3个月治疗组的5年OS率为92.7% (95% CI, 89.5 - 95.0), 6个月治疗组的5年OS率为91.8% (95% CI, 88.4 - 94.3) (HR, 0.86;95% CI, 0.53 ~ 1.37;P=0.52);对于高危患者,3个月治疗组的5年生存率为79.8% (95% CI, 74.6 - 84.0), 6个月治疗组的5年生存率为79.8% (95% CI, 74.7 - 84.1) (HR, 0.96;95% CI, 0.68 ~ 1.35;P=0.82)。
根据风险组和方案进行的OS分析提示,对于低危患者,3个月mFOLFOX6治疗可能比6个月mFOLFOX6治疗的预后更差(HR, 1.26;95% CI, 0.54 ~ 2.94;P=0.60),而3个月的CAPOX治疗似乎优于6个月的CAPOX治疗(HR, 0.71;95% CI, 0.40 ~ 1.26;P=0.24)。对于高危患者,mFOLFOX6(HR, 0.91;95% CI, 0.50 ~ 1.65;P=0.75)和CAPOX (HR, 0.99;95% CI, 0.65 ~ 1.50;P=0.95)治疗3个月和6个月的结果相似。
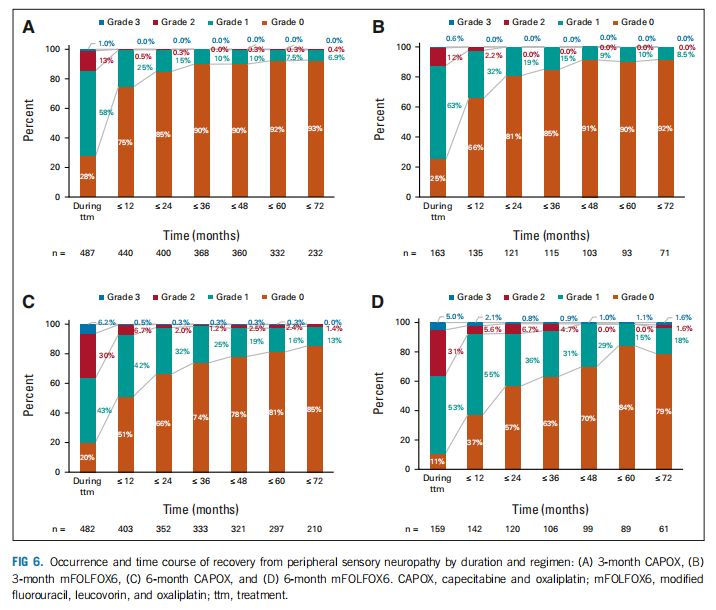
在治疗期间,3个月治疗组650例患者中有474例(73%),6个月治疗组641例患者中有526例(82%)出现任何级别的神经毒性 (OR, 0.589;95% CI, 0.451 ~ 0.768;P<0.0001)。3个月治疗组2级或3级神经毒性分别有84例(13%)和6例(1%),6个月治疗组分别有195例(30%)和38例(6%)(OR[2/3级],0.281;95% CI, 0.214 ~ 0.370;P<0.0001)。
综上,在亚洲III期结肠癌患者中,将辅助治疗时间从6个月缩短到3个月并不影响疗效,并降低了长期外周感觉神经病变的发生率。在这种情况下,3个月的CAPOX治疗是一个合适的辅助治疗选择。
原始出处:
Yoshino T, Oki E, Misumi T, Kotaka M, Manaka D, Eto T, Hasegawa J, Takagane A, Nakamura M, Kato T, Munemoto Y, Nakamura F, Bando H, Taniguchi H, Sakamoto Y, Shiozawa M, Nishi M, Horiuchi T, Yamagishi H, Sakamoto J, Mizushima T, Ohtsu A, Mori M. Final Analysis of 3 Versus 6 Months of Adjuvant Oxaliplatin and Fluoropyrimidine-Based Therapy in Patients With Stage III Colon Cancer: The Randomized Phase III ACHIEVE Trial. J Clin Oncol. 2022 May 5:JCO2102628. doi: 10.1200/JCO.21.02628. Epub ahead of print. PMID: 35512259.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











#疗效和安全性#
42
#JCO#
56
#III#
47
#铂#
49
#III期#
42