Otol Neurotol:双侧同时植入人工耳蜗后的前庭功能情况
2021-05-27 AlexYang MedSci原创
由于噪音中听觉和空间定位的优势,目前双侧人工耳蜗(CI)在重度听力损失的患者中十分受欢迎。
由于噪音中听觉和空间定位的优势,目前双侧人工耳蜗(CI)在重度听力损失的患者中十分受欢迎。
近期,有研究人员调查了双侧同步CI接受者的前庭功能情况。
研究是一项回顾性分析,在大学医院中进行。包括了16名重度听力损失的患者。研究人员在术前和术后4个月,用客观和主观的方法评估了受试者的前庭功能,并对对术前和术后的差异进行了分析。
术前的前庭测试显示,8名受试者(50%)的冷热试验测试结果异常,11只耳朵(34.4%)的眼前庭诱发肌源性电位结果异常,6只耳朵(18.8%)的颈前庭诱发肌源性电位结果异常。前半规管的7只耳朵(21.9%)和后半规管的6只耳朵(18.8%)有增益损失。然而,手术明显减少了冷热试验测试的最大慢相速度之和(p<0.05)。颈前庭诱发的肌源性电位异常率在手术后显著增加到53.1%(p<0.05)。另外,所有患者术后的眼前庭诱发肌源性电位、视频头脉冲检查(vHIT)和眩晕障碍量表(DHI)的变化都不明显。更多的是,诊断为大前庭导水管综合征患者的DHI得分明显高于其他患者(P<0.05)。Spearman相关分析显示,DHI与vHIT所证明的半规管功能障碍有中等程度的相关性(r = 0.702; p<0.001),与冷热测试结果有弱相关性(r=0.352; p=0.048)。然而,DHI和VEMPs之间没有发现相关关系。单音节和双音节单词识别得分均得到了改善,分别从0到60.4±14.3%(P<0.05)和从0到63.3±14.5%(P<0.05),然而,词汇识别得分的提高与前庭测试的变化没有相关性。
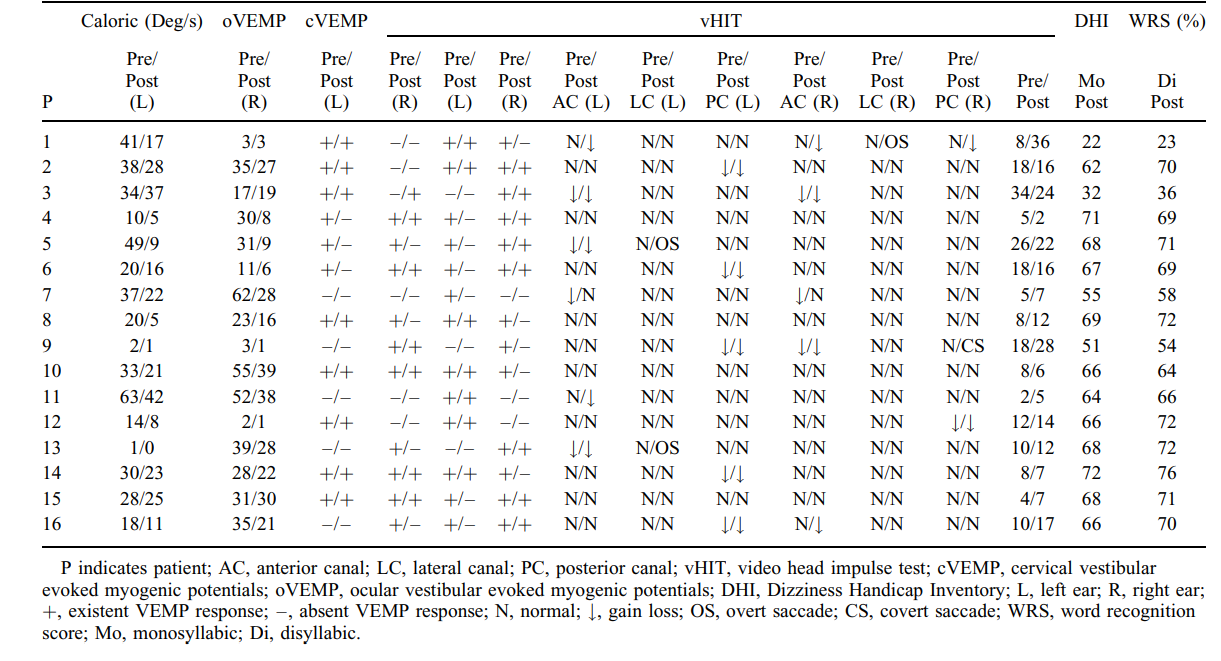
术前和术后的前庭测试、DHI评分和单词识别得分结果情况
综上所述,双侧同时进行CI后保留了椭圆囊功能以及高频下的前庭功能。然而,手术明显影响了前庭的低频功能和小囊功能。大前庭导水管综合征患者的DHI评分明显高于其他患者。DHI与vHIT适度相关,与热量弱相关。
原始出处:
Tao Yan, Fangru Zong, Xiao Han et al. Vestibular Function After Bilateral Simultaneous Cochlear Implantation. Otol Neurotol. Jun 2021
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言













#人工耳蜗#
46
#植入#
27
#双侧#
37
#前庭功能#
46