European Radiology:在低级别胶质瘤中识别IDH突变和ATRX表达缺失的放射组学列线图
2022-05-02 shaosai MedSci原创
MRI作为一种非侵入性影像学技术,被常规用于诊断和绘制胶质瘤。有研究表明,MRI和放射组学的结合可以预测胶质瘤的等级和分子亚型。
胶质瘤是最常见的恶性原发性脑肿瘤。根据2016年更新的WHO中枢神经系统肿瘤分类(2016 WHO CNS),低级别胶质瘤(LrGG,2016 WHO II-III级胶质瘤)的诊断结合了组织学特征和分子学结果,包括基于表型和基因型的异柠檬酸脱氢酶(IDH)突变状态和1p/19q编码状态。LrGG患者的预后与IDH的突变状态密切相关。IDH+LrGG,主要是R132H突变(约80%),比IDH-LrGG进展更慢,预后更好。IDH突变(IDH +)的LrGG患者的中位生存时间(7.4年)明显长于IDH野生型(IDH-)的LrGG和胶质母细胞瘤。IDH+LrGG患者可以从基于替莫唑胺的标准化疗中获益更多,对放射治疗高度敏感,也是通过IDH1 +抑制剂进行靶向治疗的合适人选。因此,识别IDH突变状态可以直接影响LrGG患者的预后评估和治疗决策。
ATRX基因突变(ATRX蛋白表达缺失,ATRX-)与替代性延长端粒(ALT)途径的激活有关,它是维持肿瘤细胞不死的重要途径之一,在IDH+胶质瘤中识别ATRX-状态可以进一步指导具体的分类和诊断,并能更准确地预测预后和进行个体化治疗。
然而,基因亚型评估依赖于手术切除和活检等侵入性方法,相当大的空间和时间异质性不可避免地降低了采样的准确性。因此,需要一种非侵入性的方法来检测IDH和ATRX突变,为LrGG患者制定个性化的干预措施。MRI作为一种非侵入性影像学技术,被常规用于诊断和绘制胶质瘤。有研究表明,MRI和放射组学的结合可以预测胶质瘤的等级和分子亚型。
然而,由于放射组学包括大量有用的定量信息,因此在受试者或患者之间比较所有选定的放射组学特征将是一种挑战。列线图是一项定量且直观的评估工具,适合在决策过程中结合放射组学特征和临床风险因素进行评估。
近日,发表在European Radiology杂志的一项研究提出了一个预测LrGG患者IDH和ATRX突变状态的列线图,为临床医生提供了一个对LrGG患者的IDH和ATRX突变状态进行无创分层的易于使用且更准确的影像学工具。
本研究共纳入111名LrGG患者(76名IDH突变型和35名IDH野生型),分为训练集(n = 78)和验证集(n = 33)用于预测IDH突变。IDH + LrGG患者被进一步分层为ATRX-(n = 38)和ATRX +(n = 38)亚型。从每个肿瘤的感兴趣区域共提取了250个放射组学特征,包括来自T2FLAIR、增强T1WI、CBF、ADC和指数ADC(eADC)。使用弹性网回归模型选择了放射组学特征,并利用年龄、性别信息和上述特征最终构建了放射组学列线图。
放射组学列线图实现了对IDH突变(C-index:训练集=0.881,验证集=0.900)和ATRX缺失(C-index:训练集=0.863,验证集=0.840)LrGG患者的识别,具有良好的校准性。决策曲线分析进一步证实了这两个列线图对预测IDH和ATRX状态的临床作用。
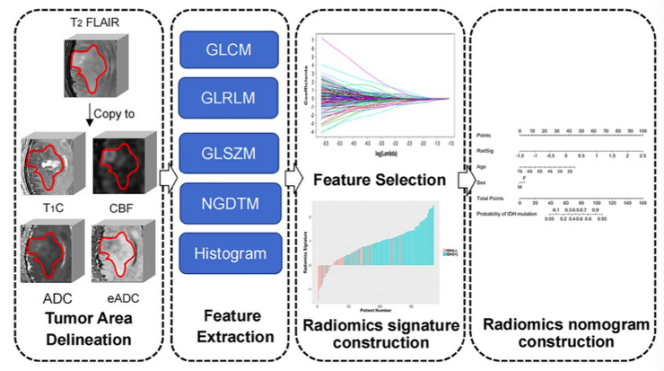
图 确定低级别胶质瘤IDH和ATRX突变状态的列线图策略示意图
总之,结合年龄、性别和放射组学特征的列线图为预测LrGG患者的IDH和ATRX突变提供了一种非侵入性的影像学方法,这可以协助临床进行个性化治疗方案的制定。
原文出处:
Shiman Wu,Xi Zhang,Wenting Rui,et al.A nomogram strategy for identifying the subclassification of IDH mutation and ATRX expression loss in lower-grade gliomas.DOI:10.1007/s00330-021-08444-1
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











#列线图#
38
#PE#
40
#胶质瘤##放射组学#
74
#低级别胶质瘤#
37
#ATRX#
30
很前沿的咨询,谢谢分享!!!
59