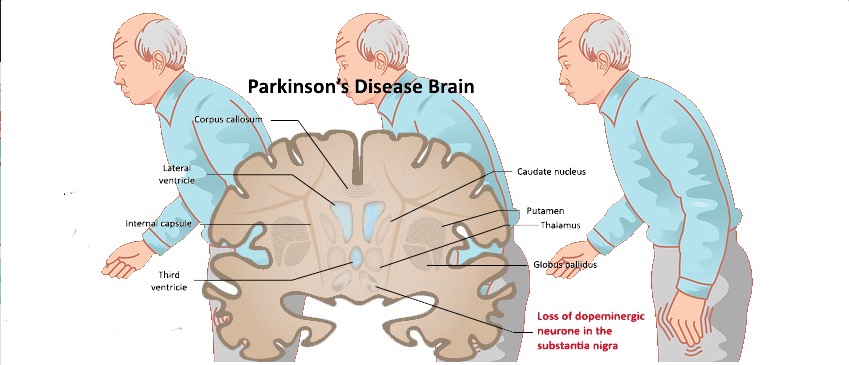
帕金森病(PD)是第二种最常见的神经退行性疾病,其发病率在男性中比女性高1.5至2.0倍。雌激素已被证明具有神经保护作用,特别是通过增加多巴胺的合成、神经营养因子的上调、防止路易体的形成和α-突触核蛋白的聚集,对黑质通路具有保护作用。
雌激素还具有抗氧化和抗炎特性,通过降低细胞因子和其他炎症调节剂的水平。基于这些临床和实验观察,有人假设荷尔蒙暴露可能对妇女的PD有保护作用。然而,关于雌激素在PD中的作用的数据仍然是矛盾的,特别是关于绝经年龄和绝经类型的作用。
藉此,法国Paris-South University的Marianne Canonico等人,利用PARTAGE病例对照研究的数据,探究了荷尔蒙暴露(绝经年龄和绝经类型、绝经后荷尔蒙治疗)与PD的关联。并区分手术绝经和早期绝经年龄对PD的影响。
该PARTAGE病例对照包括130名女性病例和255名年龄匹配的女性对照。妇科病史的信息通过标准化的调查问卷采集,PD通过神经系统检查进行验证。最后使用条件逻辑回归法计算(ORs)。
他们发现:在调整了教育水平、吸烟状况、职业上接触杀虫剂以及喝咖啡和酒之后,早期双侧输卵管切除的妇女的关联最显著(OR=4.61;95%CI=2.22-9.56)。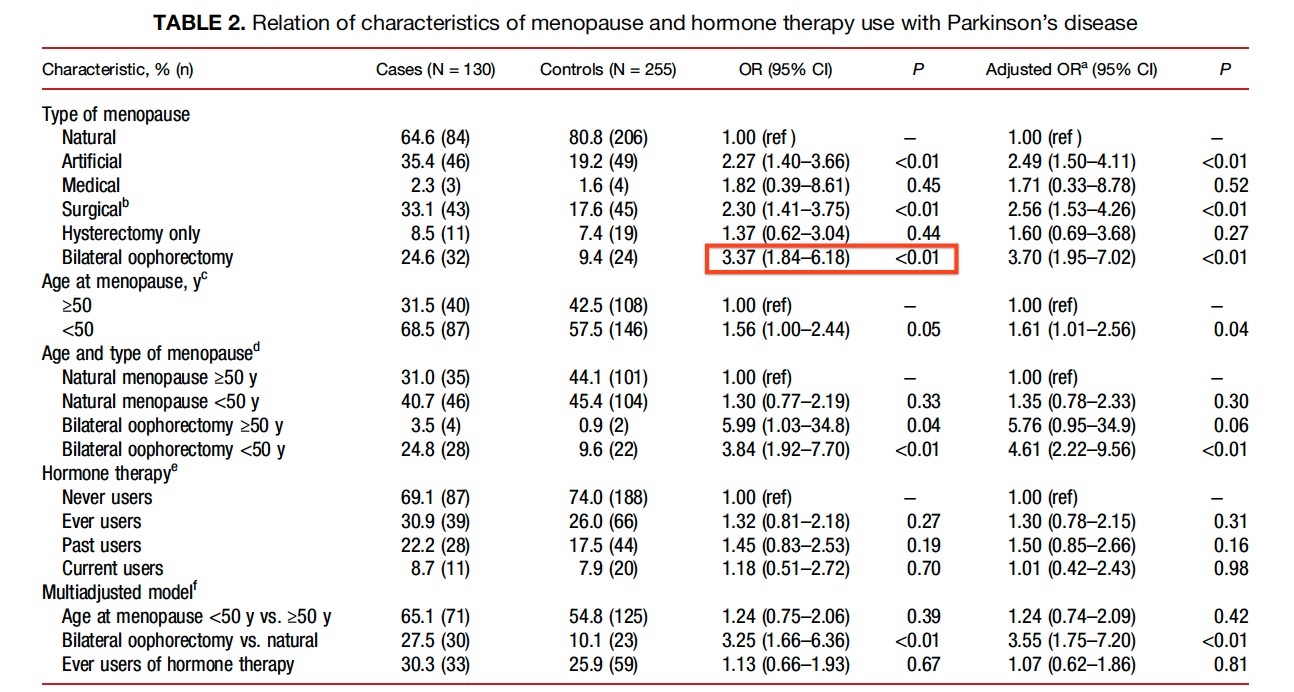
双侧卵巢切除术和绝经年龄之间没有明显的交互作用,50岁前和50岁后的双侧卵巢切除术之间没有明显的差异(P=0.59)。
此外,50岁之前绝经(OR=1.24,95%CI=0.74-2.09)或激素治疗(HT;OR=1.07,95%CI=0.62-1.86)都与PD有关。
这个研究的重要意义在于发现了:双侧输卵管切除术与PD的风险增加有关。
原文出处;
Canonico M, Pesce G, Bonaventure A, et al. Increased Risk of Parkinson’s Disease in Women after Bilateral Oophorectomy. _Mov Disord_. 2021;36(7):1696-1700. doi:10.1002/mds.28563.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#切除术#
33
#卵巢切除术#
35
#Dis#
26
#Disord#
22
#双侧#
36