Nature:麻省理工学院冯国平团队揭示帕金森病治疗新靶点,靶向丘脑回路可挽救帕金森病运动和情绪缺陷
2022-06-11 小柯生命 小柯生命
药物治疗(L-多巴)和脑深部电刺激是目前治疗帕金森病的主要手段,可以有效地改善肢体震颤等运动症状,但是对于非运动症状,例如情绪紊乱收效甚微。
帕金森病是一种常见的神经退行性疾病,传统上认为帕金森病是一种运动系统疾病,最明显的为运动功能减退,颤抖,肢体僵硬。但现在认为,帕金森其实是一种具有多种临床特征的复杂疾病,除了运动症状外,其临床症状还包括神经精神性及其他非运动表现,例如情绪紊乱,睡眠紊乱等等。
药物治疗(L-多巴)和脑深部电刺激是目前治疗帕金森病的主要手段,可以有效地改善肢体震颤等运动症状,但是对于非运动症状,例如情绪紊乱收效甚微。因此,对于帕金森病中运动以及非运动症状机制的研究,可以为帕金森病的治疗提供新思路以及新靶点。
2022年6月8日,美国麻省理工学院冯国平教授团队(张颖博士和 Dheeraj Roy 博士为论文共同第一作者)在国际顶尖学术期刊 Nature 上发表了题为:Targeting thalamic circuits rescues motor and mood deficits in PD mice 的研究论文 。
通过对丘脑环路的研究,冯国平团队首次揭示了帕金森病中运动以及非运动症状的治病机制,发现了新的可以用于帕金森治疗的药物靶点。靶向丘脑回路可挽救帕金森病模型小鼠的运动和情绪缺陷。
Parafascicular thalamus(PF)是丘脑板内核群的重要组成部分,因为与运动基底核团的密切联系,一般被认为是一个运动相关的丘脑核团。在帕金森患者的脑部也可以检测到PF神经元大量特异性的衰退。因为缺乏特异有效的操作手段,PF 在以往的研究中长期被忽略,其行为学功能,特别是其在帕金森病中的致病机制,并不明确。
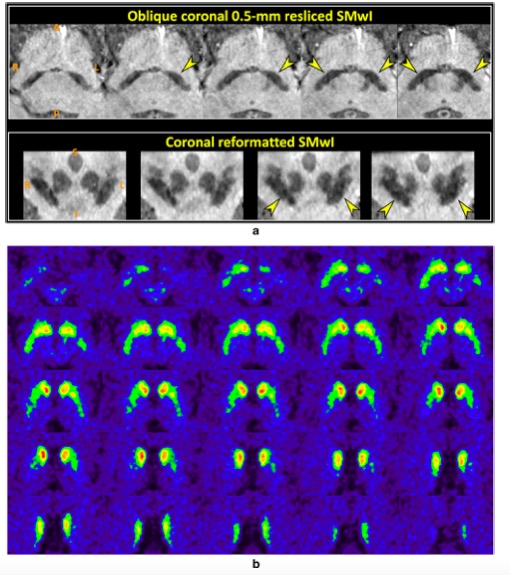
通过新颖的环路操控技术以及在体钙成像的方法,研究团队首先研究了野生型小鼠中 PF 环路及其功能,第一次发现了 PF 中存在三种不同的神经元亚群:一类 PF 神经元投射到背侧纹状体 CPu(Caudate Putamen)调节运动功能;一类 PF 神经元投射到丘脑下核 STN(Subthalamic nucleus)调控运动学习功能;还有一类 PF 神经元可以投射到腹侧纹状体NAc(Nucleus accumbens)参与抑郁样行为的产生。有意思的是,通过进一步对 PF→STN 环路的研究,研究团队发现在 STN 中发现了一群兴奋性投射的 PV 神经元,而就是这群神经元参与了运动学习的功能。
运动功能减退,运动学习能力的降低,以及抑郁样行为都是帕金森疾病的症状,那么,这些不同的 PF 神经元亚群及其环路是否参与了帕金森的致病呢?通过对帕金森病小鼠模型的研究,研究人员发现三种不同的 PF 环路均存在不同程度的异常:PF→CPu 环路在帕金森病小鼠中突触连接增强;PF→STN 环路在帕金森病小鼠中突触可塑性降低;PF→NAc 环路在帕金森病小鼠中突触连接减弱。
那么,如果特异性地调控帕金森病模型小鼠中不同的 PF 环路,能不能有效改善帕金森病的症状呢?研究团队发现,用药理学遗传的方法特异性抑制投射到 CPu 的 PF 神经元,可以长期改善小鼠的运动功能。用光遗传的方法增强 PF→NAc 环路的突触可塑性可以有效改善帕金森病小鼠的运动学习功能。通过在 NAc 投射的 PF 神经元中表达一种新型的光敏感蛋白 SOUL,研究人员可以用非损伤的方法改善帕金森病小鼠的抑郁样行为。
通过光遗传以及药理学遗传的方法,研究人员可以有效改善帕金森病模型小鼠的运动以及非运动症状。接下来,研究人员想知道,能不能在不同的 PF 环路中找到各自的药物学分子靶点,从而起到治疗的作用的呢?
通过一系列研究,他们发现,不同的乙酰胆碱受体可以表达在不同的 PF 环路中,使用其特异性的激动剂或者拮抗剂可以有效改善帕金森病小鼠的运动功能,运动学习功能,以及抑郁样行为。值得一提的是,通过对猕猴的研究,研究人员证实,这些乙酰胆碱受体也在灵长类动物的 PF 环路中特异性表达。
该研究通过对单一丘脑核团的调控同时改善了帕金森病的运动以及非运动症状,同时揭示了相应的分子靶点,为帕金森病的治疗提供新思路以及新方向。
原始出处:
Zhang, Y., Roy, D.S., Zhu, Y. et al. Targeting thalamic circuits rescues motor and mood deficits in PD mice. Nature (2022). https://doi.org/10.1038/s41586-022-04806-x.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#脑回路#
49
#Nat#
0
#新靶点#
31
#治疗新靶点#
46
#丘脑#
53
#丘脑#
40
学习了
54