病例分享:陈旧性前壁心梗、阵发性房颤、心尖部血栓、胸闷症状再发
2017-12-02 佚名 中国医学论坛报
患者2年前活动后感胸闷、气短,伴有干咳,无胸痛、大汗等其他不适,休息后缓解,劳累后加重,未规则诊治。
病例提供者:王汝涛西京医院
患者,男,51岁。主诉:发作性胸闷、气短、干咳2年,加重12天。
现病史
患者2年前活动后感胸闷、气短,伴有干咳,无胸痛、大汗等其他不适,休息后缓解,劳累后加重,未规则诊治。
此次入院前12天,患者自觉干咳加重,当地医院行胸部CT显示:双肺炎症伴少量胸腔积液;心脏彩超:陈旧性心梗,左室大,心尖部血栓;冠脉CTA:LAD狭窄大于60%,予以抗血小板、抗凝、止咳、抗感染等治疗后,症状缓解不明显。
既往史
体格检查
体温:36.2℃,脉搏:90次/分,呼吸:20次/分,血压:106/62 mmHg。双肺呼吸音清,双下肺可闻及细湿啰音,心率:90次/分,律齐,未闻及早搏,未闻及杂音。
辅助检查
Pro-BNP:4317 pg/ml,肌钙蛋白I:0.051 ng/ml,肌红蛋白:41.1 ng/ml,肌酸激酶同工酶:1.50 ng/ml。
心脏彩超:EF:39%,提示前间隔、左室前壁心肌梗死,左心室圆钝并心尖部血栓形成,左房左室大,肺动脉高压(收缩压约66 mmHg),三尖瓣轻度关闭不全。
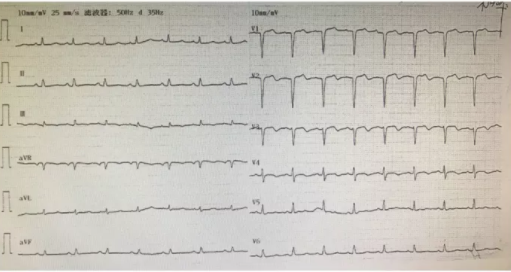
心电图:
1、冠心病,陈旧性心肌梗死,不稳定性心绞痛,心功能2级;2、阵发性房颤;3、心室血栓。
风险评分
Grace评分:107.6
Crusade评分:32,中危。
治疗经过
结合冠脉造影结果,患者三支病变,右冠发育相对较小,旋支发育粗大。虽然患者心电图提示前壁陈旧性心梗,但仔细分析造影结果,旋支病变较重,且旋支较粗大,供血范围广泛,所以首次手术策略决定首先处理旋支病变,择期处理前降支病变。
进入导丝后旋支显影不清,考虑斑块负荷重,不排除血栓形成。在术中尽量避免反复扩张及造影,我们使用2.0×20 mm预扩球囊8 atm处理旋支远段,球囊预扩张后于LCX由远及近依次植入2.5×18 mm,2.75×23 mm,3.0×23 mm药物涂层支架3枚,支架植入后并分别使用高压球囊后扩张支架内。扩张时避免反复多次扩张,以避免慢血流发生。
主要PCI过程:


术后诊治
术后用药:阿司匹林100 mg qd,氯吡格雷75 mg qd,阿托伐他汀钙20 mg qn,贝那普利5 mg qd,利伐沙班2.5 mg bid,美托洛尔缓释片23.75 mg qd,利尿剂。
1月后,患者心室血栓减小,复查冠脉造影,旋支支架内血流通畅,无再狭窄,处理左冠前降支病变,于LAD由远及近植入药物涂层支架3枚。
术后2月复查心脏彩超心室血栓消失,心功能改善,心脏较前缩小,病人无不适症状。
临床思辨
该患者三支病变,心功能下降,心尖部伴有血栓形成,有阵发性房颤病史,危险分层为中危。
患者有心尖部血栓形成,可考虑华法林或新型口服抗凝药治疗。华法林起效慢,安全窗窄,需频繁监测,而新型口服抗凝药无需监测,疗效肯定。
结合目前循证医学证据,冠心病合并房颤时,若合用新型口服抗凝药只能选择氯吡格雷,替格瑞洛尚无证据支持。
该患者采用利伐沙班联合阿司匹林、氯吡格雷安全有效,服用3月后复查心尖部血栓消失。使用利伐沙班联合阿司匹林及氯吡格雷有效的起到了抗栓疗效,且无出血并发症。患者术后9月随访病情控制良好。
点评专家
王琼副主任医师空军军医大学西京医院
点评内容
这个病例有几个方面可以改进:首先,应该考虑先抗凝,把心室内血栓尽可能溶掉,降低心腔内血栓的问题;然后,再考虑介入开通血管。
该病例有陈旧性心梗和阵发性房颤病史,这次疾病发作需要考虑是由于心衰还是由于心梗引起,明确病因。实验室检查显示,肌酸激酶及同工酶都没有升高,只有BNP高,说明发作是由于心衰。
这个病例的亮点在于,给临床提供了一个很好的冠心病合并有阵发性房颤,同时有心室血栓形成的例子。这部分患者在抗凝、抗血小板的过程中,需要非常谨慎的用药,以最大程度的消除血栓,预防左心耳血栓的形成,同时减少出血并发症。
该病例用药,可考虑先用利伐沙班高剂量,使血栓在1到2月内消除,然后再介入治疗;介入后维持阿司匹林、氯吡格雷以及小剂量利伐沙班的长期应用。
该病例开通血管后的用药则非常标准规范,还有几个问题需要注意:1、什么时候进行血运重建:可考虑先改善心衰,并抗凝一段时间后再进行血运重建。2、针对该病例,介入先处理哪条血管:患者有陈旧性前壁心梗病史,处理前降支以及回旋支都是必要的,从风险角度来看先做前降支是比较安全的做法。3、合并房颤的患者,氯吡格雷是抗血小板治疗的最佳选择,指南唯一推荐。
用药小贴士
2017年ESC新版冠脉疾病的双联抗血小板治疗指南中指出:氯吡格雷是首选应用于PCI治疗稳定型冠心病患者、需联合应用口服抗凝治疗患者和禁用替格瑞洛或普拉格雷(如存在颅内出血风险)ACS患者的P2Y12抑制剂。
对于有口服抗凝治疗指征的患者(存在高缺血风险,或其他解剖学特征使得缺血风险高于出血风险),应考虑应用三联抗栓治疗(阿司匹林、氯吡格雷和OAC)1至6个月。同时不建议在这类患者中使用替格瑞洛或普拉格雷。
小提示:本篇资讯需要登录阅读,点击跳转登录
版权声明:
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言






#心尖#
35
#胸闷症状再发#
28
#胸闷#
42
#阵发性房颤#
40
#陈旧性#
32
学习了受益匪浅
60